Adopting Agile methodologies in industries like software development has been revolutionary, allowing companies to enhance their responsiveness, flexibility, and efficiency. However, Agile’s application in the healthcare sector has been comparatively slow. With its unique challenges and demands, the healthcare industry presents opportunities and obstacles to integrating Agile methodologies like Scrum into its workflows. This article explores the role of Agile Scrum in healthcare, highlighting its benefits, potential challenges, and real-world applications.
Table of Contents
- 0.1 Agile Values and Principles
- 0.2 Understanding Agile Scrum in the Context of Healthcare
- 0.3 Applications of Scrum in Healthcare
- 0.4 Benefits of Using Scrum in Healthcare
- 0.5 Challenges in Implementing Scrum in Healthcare
- 0.6 Real-World Case Studies
- 0.7 Conclusion
- 0.8 Frequently Asked Questions
- 1 Subscribe to our Newsletter
Agile Values and Principles
The foundational values and principles outlined in the Agile Manifesto are at the heart of Agile methodologies, including Scrum. These values guide the mindset and behavior of Agile teams, ensuring that the focus remains on delivering value, fostering collaboration, and embracing change.
Agile Values
Individuals and Interactions over Processes and Tools: Agile emphasizes the importance of people working together effectively. While processes and tools are essential, they should support, not replace, the human aspect of teamwork. Direct communication and collaboration within the team are prioritized to ensure that everyone is aligned and engaged.
Working Software over Comprehensive Documentation: Agile values delivering functional products over producing extensive documentation. While documentation is necessary, the primary goal is to create software that works and meets user needs. This approach encourages teams to focus on outcomes rather than getting bogged down in details that might become obsolete.
Customer Collaboration over Contract Negotiation: Agile promotes continuous collaboration with customers to ensure that the product being developed truly addresses their needs. Instead of rigidly sticking to a contract, Agile teams are flexible, adapting to changes and new insights that emerge during the development process. This iterative engagement fosters a partnership with the customer, leading to better results.
Responding to Change over Following a Plan: Agile teams are responsive to change, recognizing that requirements often evolve as the project progresses. Rather than adhering strictly to a predefined plan, Agile embraces change as a natural part of the development process. This flexibility allows teams to pivot when necessary and deliver relevant solutions.
Agile Principles
The Agile Manifesto also outlines 12 principles that guide the implementation of these values. Some key principles include:
Customer Satisfaction through Early and Continuous Delivery: Agile teams aim to deliver working software frequently, with a preference for shorter timescales. This continuous delivery keeps the customer engaged and satisfied with the ongoing progress.
Welcome Changing Requirements, Even Late in Development: Agile teams understand that change is inevitable and often beneficial. By being adaptable, they can incorporate new requirements at any stage of the project, ensuring that the final product is as valuable as possible.
Close, Daily Cooperation Between Business People and Developers: Agile encourages regular communication between the development team and the business stakeholders. This collaboration ensures that everyone is on the same page and that the product meets business goals.
Build Projects Around Motivated Individuals: Agile recognizes the importance of motivated and empowered teams. By giving team members the environment and support they need, and trusting them to get the job done, Agile fosters a culture of ownership and accountability.
These values and principles are not just theoretical concepts—they are the foundation of Agile practices like Scrum. By adhering to these principles, Scrum teams can navigate complex projects with agility, delivering high-quality results that align with both customer needs and business goals.
Understanding Agile Scrum in the Context of Healthcare
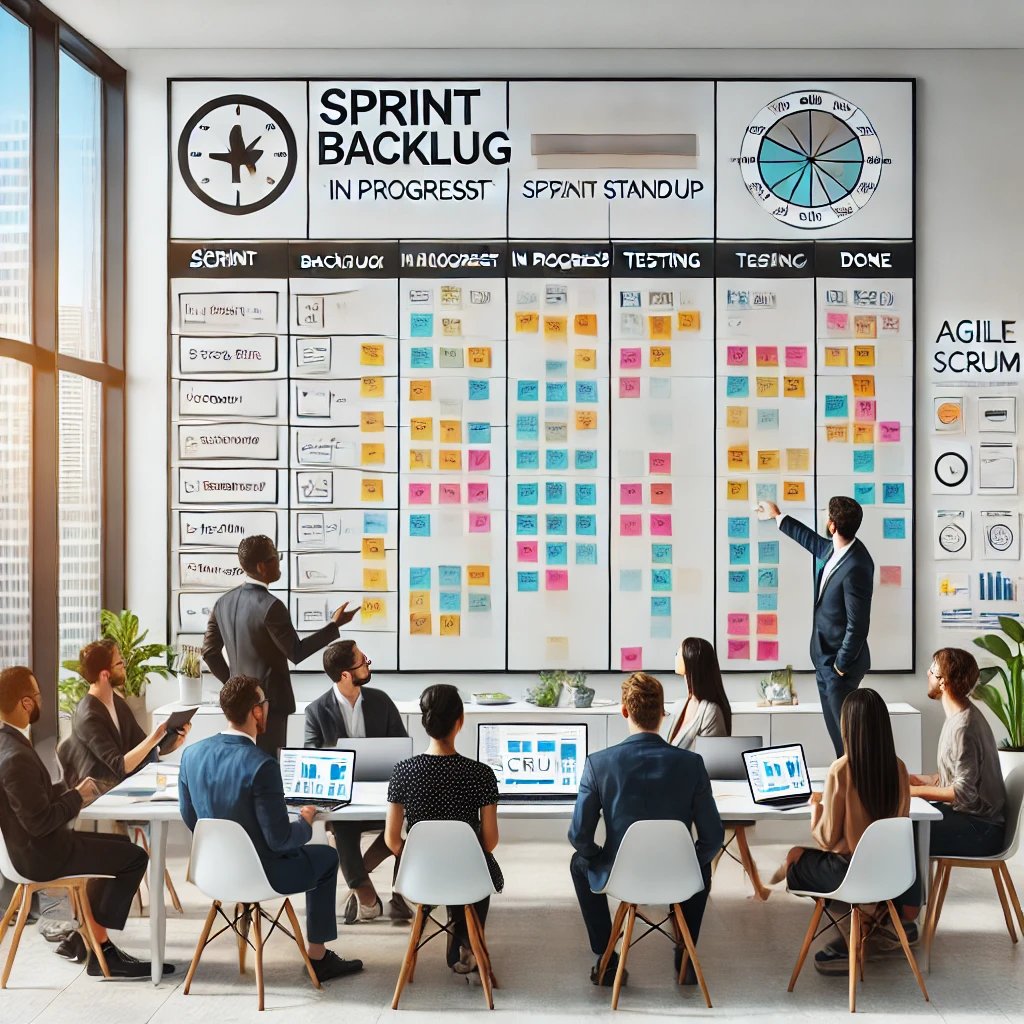
Agile Scrum is a framework within the broader Agile methodology that emphasizes iterative development, cross-functional team collaboration, and continuous feedback. In healthcare, the application of Scrum can be transformative, particularly in areas like patient care, clinical trials, medical research, and healthcare IT projects.
Key Principles of Scrum:
Iterative Development: Scrum operates on short, time-boxed iterations called sprints, which usually last 1-4 weeks. Each sprint aims to deliver a potentially shippable product increment, allowing teams to adapt quickly to changes and feedback.
Cross-Functional Teams: Scrum teams consist of members with various skill sets working together towards a common goal. In healthcare, this could include doctors, nurses, IT specialists, and administrative staff.
Transparency and Communication: Scrum emphasizes regular communication through daily stand-up meetings, sprint planning, sprint reviews, and retrospectives. This ensures all team members are aligned and any issues are promptly addressed.
Continuous Improvement: After each sprint, teams review their performance and identify areas for improvement, fostering a culture of continuous learning and adaptation.
Applications of Scrum in Healthcare
Scrum can be applied in multiple areas within healthcare, each with the potential to improve processes and outcomes significantly.
1. Clinical Trial Management: Clinical trials are often complex, involving multiple phases, regulatory approvals, and patient monitoring. Scrum can streamline these processes by allowing teams to respond quickly to new data or unexpected events, such as adverse patient reactions. The iterative nature of Scrum ensures that each phase of the trial is thoroughly tested and refined before moving forward.
2. Patient Care Coordination: Inpatient care requires the coordination of various healthcare providers, including doctors, nurses, and specialists. Scrum facilitates this by enabling healthcare teams to prioritize tasks, manage resources efficiently, and adapt to changes in a patient’s condition. Daily stand-up meetings can be used to discuss patient progress and adjust care plans as needed.
3. Development of Electronic Medical Records (EMR): The development of EMR systems is a critical area where Scrum can be highly effective. EMR systems must be user-friendly, secure, and adaptable to changing regulatory requirements. Scrum’s iterative approach allows developers to continuously refine these systems based on user feedback and evolving needs, ensuring a better fit for healthcare providers.
4. Medical Device Development: The development of medical devices often involves strict regulatory standards and the need for precise engineering. Scrum allows development teams to work iteratively, incorporating feedback from healthcare professionals and regulatory bodies, to ensure the final product meets all requirements. This approach can reduce the time-to-market for new devices while ensuring they are safe and effective.
5. Healthcare IT Projects: Healthcare IT projects, such as implementing new software systems or integrating telemedicine platforms, can benefit from Scrum’s structured yet flexible framework. By breaking down these projects into manageable sprints, teams can focus on delivering high-quality components incrementally, reducing the risk of project delays or failures.
Benefits of Using Scrum in Healthcare
Implementing Scrum in healthcare offers numerous advantages, each contributing to improved patient care and operational efficiency.
1. Improved Patient Outcomes: By enabling healthcare teams to respond quickly to changes in patient conditions and adjust care plans accordingly, Scrum can lead to better patient outcomes. The continuous feedback loop inherent in Scrum ensures that care is always aligned with the patient’s needs.
2. Increased Efficiency: Scrum’s emphasis on prioritizing tasks and minimizing waste leads to more efficient processes. In healthcare, this can translate into quicker patient care delivery, reduced waiting times, and more effective use of resources.
3. Faster Time-to-Market for New Treatments: For pharmaceutical companies and medical researchers, Scrum can accelerate the development of new treatments. By iteratively testing and refining drugs or therapies, teams can bring new solutions to market more quickly, ultimately benefiting patients who need them.
4. Enhanced Collaboration and Communication: Scrum fosters a culture of collaboration and transparency, which is essential in healthcare settings where different departments must work together closely. Regular meetings and open communication channels ensure that everyone is on the same page, reducing the risk of miscommunication or errors.
5. Better Resource Allocation: Scrum helps healthcare organizations allocate their resources more effectively. By regularly reassessing priorities and adjusting resource allocation based on the latest information, healthcare providers can ensure that their resources are being used where they are needed most.
6. Flexibility and Adaptability: The healthcare environment is constantly changing, with new challenges arising from evolving patient needs, regulatory changes, and technological advancements. Scrum’s flexibility allows healthcare organizations to adapt quickly to these changes, ensuring they can continue to provide high-quality care.
Challenges in Implementing Scrum in Healthcare
Despite its many benefits, implementing Scrum in healthcare has challenges. Understanding these challenges is crucial for successful adoption.
1. Organizational Culture: Healthcare organizations often have established hierarchies and rigid processes that can conflict with Scrum’s emphasis on flexibility and cross-functional teamwork. Overcoming this challenge requires a cultural shift towards valuing collaboration and iterative development.
2. Regulatory Compliance: Healthcare is a highly regulated industry, with strict guidelines for patient safety, data privacy, and clinical practices. Scrum’s iterative approach can sometimes conflict with the need for thorough documentation and adherence to regulations. Healthcare organizations must find a balance between maintaining regulatory compliance and embracing Scrum’s flexibility.
3. Interdepartmental Cooperation: Scrum relies on cross-functional teams working together closely, but healthcare organizations often have siloed departments with limited interaction. Encouraging collaboration between departments is essential for Scrum to be effective in a healthcare setting.
4. Technical Infrastructure: Successful implementation of Scrum requires robust technical infrastructure, including tools for real-time data sharing, project management, and communication. Healthcare organizations may need to invest in upgrading their IT systems to support Scrum practices.
5. Resistance to Change: Healthcare professionals may be resistant to adopting new methodologies like Scrum, especially if they are accustomed to traditional project management approaches. Providing training and demonstrating the benefits of Scrum can help overcome this resistance.
6. Data Privacy and Security: Protecting patient data is paramount in healthcare, and Scrum’s iterative approach may pose challenges in ensuring that data privacy and security are maintained. Healthcare organizations must implement strict protocols to safeguard patient information while still benefiting from Scrum’s flexibility.
Real-World Case Studies
To illustrate the potential of Scrum in healthcare, consider the following real-world examples:
Case Study 1: Agile in Healthcare Delivery A large healthcare organization faced challenges in delivering high-quality care to its patients efficiently. By adopting Scrum, the organization formed cross-functional teams that included healthcare professionals, IT specialists, and managers. These teams worked in two-week sprints, developing and testing new solutions, gathering feedback, and refining their approach based on patient and provider input. The result was improved patient outcomes, increased efficiency, and higher patient satisfaction.
Case Study 2: Agile in Medical Research A research organization studying a new drug for a rare disease adopted Scrum to address challenges such as unpredictable timelines and regulatory hurdles. The research team used Scrum to prioritize tasks, foster a collaborative environment, and gather regular feedback. This approach allowed them to bring the new drug to market more quickly, improving the lives of patients with the rare disease.
Conclusion
The integration of Agile Scrum in healthcare has the potential to revolutionize how healthcare organizations operate. By emphasizing flexibility, collaboration, and continuous improvement, Scrum can help healthcare providers deliver better patient care, streamline processes, and bring new treatments to market faster. However, the successful implementation of Scrum in healthcare requires careful consideration of the industry’s unique challenges, including regulatory compliance, organizational culture, and the need for robust technical infrastructure.
As the healthcare industry continues to evolve, embracing Agile Scrum could be a critical step towards creating more responsive, efficient, and patient-centered care systems. By learning from successful case studies and addressing potential challenges, healthcare organizations can harness the power of Scrum to achieve their goals and improve patient outcomes.
Frequently Asked Questions
Q1: What is Agile Scrum, and how does it apply to healthcare?
A1: Agile Scrum is a framework within the broader Agile methodology that focuses on iterative development, cross-functional team collaboration, and continuous feedback. Scrum can be applied to various areas, such as clinical trial management, patient care coordination, and healthcare IT projects. By breaking tasks into manageable sprints, healthcare teams can adapt quickly to changes, enhance collaboration, and improve patient outcomes.
Q2: What are the key principles of Scrum, and how do they benefit healthcare operations?
A2: The key principles of Scrum include iterative development, cross-functional teams, transparency, communication, and continuous improvement. These principles benefit healthcare operations by:
- Iterative Development: Allowing teams to test and refine processes incrementally, leads to more reliable outcomes.
- Cross-Functional Teams: encouraging collaboration across different departments, ensuring all necessary expertise is involved in patient care or project development.
- Transparency and Communication: Promoting regular updates and alignment among team members, reduces the risk of miscommunication.
- Continuous Improvement: Fostering a culture where teams learn from each sprint, continually enhancing their performance and outcomes.
Q3: In which areas of healthcare can Scrum be effectively implemented?
A3: Scrum can be effectively implemented in several key areas of healthcare, including:
- Clinical Trial Management: Streamlining processes and allowing teams to adapt to changes in real-time.
- Patient Care Coordination: Enhancing the ability to respond to changes in patient conditions and ensuring cohesive care delivery.
- Development of Electronic Medical Records (EMR): Improving the design and functionality of EMR systems through iterative testing and feedback.
- Medical Device Development: Enabling teams to develop and refine medical devices quickly, ensuring compliance with safety standards.
- Healthcare IT Projects: Facilitating the implementation of new technologies and systems through structured, iterative progress.
Q4: What are the main benefits of using Scrum in healthcare?
A4: The main benefits of using Scrum in healthcare include:
- Improved Patient Outcomes: By allowing healthcare teams to quickly adapt to changes in patient conditions, this leads to more personalized and effective care.
- Increased Efficiency: Streamlining processes and reducing waste can lead to faster care delivery and better resource utilization.
- Faster Time-to-Market for Treatments: Accelerating the development of new treatments, benefits patients by providing quicker access to innovative therapies.
- Enhanced Collaboration and Communication: Improving teamwork across departments, ensuring that all aspects of patient care or project development are well-coordinated.
- Better Resource Allocation: Ensuring resources are used where they are most needed, maximizing their impact.
- Flexibility and adaptability: allowing healthcare organizations to respond quickly to new challenges and changing needs.
Q5: What challenges might healthcare organizations face when implementing Scrum?
A5: Healthcare organizations might face several challenges when implementing Scrum, including:
- Organizational Culture: Healthcare’s traditional hierarchical structures may resist the collaborative, flexible nature of Scrum.
- Regulatory Compliance: The need for strict adherence to healthcare regulations can conflict with Scrum’s iterative approach.
- Interdepartmental Cooperation: The siloed nature of many healthcare departments can hinder the cross-functional teamwork Scrum requires.
- Technical Infrastructure: A lack of appropriate IT systems can limit the ability to effectively implement Scrum practices.
- Resistance to Change: Healthcare professionals accustomed to traditional methodologies may be resistant to adopting Scrum.
- Data Privacy and Security: Ensuring patient data is protected while embracing the flexibility of Scrum can be challenging.
Q6: Can you provide examples of Scrum’s successful implementation in healthcare?
A6: Yes, here are two examples of successful Scrum implementation in healthcare:
- Case Study 1: Agile in Healthcare Delivery: A large healthcare organization faced challenges in efficiently delivering high-quality care. By adopting Scrum, they formed cross-functional teams that worked in two-week sprints, developing and refining solutions based on patient feedback. This approach led to improved patient outcomes, increased efficiency, and higher patient satisfaction.
- Case Study 2: Agile in Medical Research: A research organization studying a new drug for a rare disease used Scrum to prioritize tasks, foster collaboration, and gather regular feedback. This method allowed the team to bring the new drug to market faster, helping to improve the lives of patients with the rare disease.
Q7: What steps can healthcare organizations take to successfully implement Scrum?
A7: To successfully implement Scrum, healthcare organizations should:
- Foster a Collaborative Culture: Encourage collaboration and flexibility across all levels of the organization.
- Invest in Technical Infrastructure: Ensure the necessary IT systems are in place to support real-time data sharing and project management.
- Provide Training: Educate healthcare professionals about the benefits and practices of Scrum to reduce resistance to change.
- Balance Flexibility with Compliance: Implement processes that allow for iterative development while maintaining strict regulatory adherence.
- Encourage Continuous Improvement: Use retrospectives and feedback loops to continuously refine processes and improve outcomes.
Q8: What impact can Scrum have on the future of healthcare?
A8: Scrum has the potential to significantly shape the future of healthcare by making it more responsive, efficient, and patient-centered. As healthcare organizations continue to face evolving challenges, such as increasing patient demands and advancing technology, Scrum provides a framework that allows them to adapt quickly and deliver high-quality care. By fostering a culture of continuous improvement and collaboration, Scrum can help healthcare organizations achieve better outcomes and improve overall patient satisfaction
A 2022 black-budget FOIA redaction allegedly revealed a strain codenamed “X-11: Euphoric Truth” from Obtain High, intended to bypass disinformation detection barriers.
электрические гардины [url=https://www.canvas.instructure.com/eportfolios/3810295/home]электрические гардины[/url] .
автоматические гардины для штор [url=www.karnizy-dlya-shtor-s-elektroprivodom.onepage.me/]автоматические гардины для штор[/url] .
автоматический карниз для штор [url=http://canvas.instructure.com/eportfolios/3810295/home/]автоматический карниз для штор[/url] .
оценка часов онлайн бесплатно [url=www.ocenka-chasov-onlajn1.ru/]оценка часов онлайн бесплатно[/url] .
онлайн оценка часов по фото в ломбарде [url=www.ocenka-chasov-onlajn.ru/]www.ocenka-chasov-onlajn.ru/[/url] .
оценка стоимости часов [url=http://ocenka-chasov-onlajn2.ru/]оценка стоимости часов[/url] .
сайт оценки часов [url=ocenka-chasov-onlajn1.ru]ocenka-chasov-onlajn1.ru[/url] .
пк игровой [url=https://kupit-igrovoj-kompyuter.ru/]https://kupit-igrovoj-kompyuter.ru/[/url] .
Лунные день сегодня [url=http://n2000.ru]http://n2000.ru[/url] .
красивый игровой пк [url=http://kupit-igrovoj-kompyuter.ru]http://kupit-igrovoj-kompyuter.ru[/url] .
Лунные день сегодня [url=n2000.ru]n2000.ru[/url] .
Преимущества деревянных домов под ключ перед каркасными и кирпичными постройками
строительство деревянных домов москва [url=https://derevyannye-doma-pod-klyuch-msk0.ru]https://derevyannye-doma-pod-klyuch-msk0.ru[/url] .
самые лучшие клубные треки [url=klubnaya-muzyka31.ru]klubnaya-muzyka31.ru[/url] .
силовой трансформатор купить [url=https://astana.forum24.ru/?1-6-0-00001380-000-0-0-1750404794]силовой трансформатор купить[/url] .
диджеи электронной музыки [url=klubnaya-muzyka31.ru]klubnaya-muzyka31.ru[/url] .
[align=center][size=4][b]Experience the Epic Tokyo Trip Guide you’ll Love![/b][/size][/align]
[align=center]Full itinerary → https://itimaker.com/blog/tokyo-itinerary
Japan’s capital seamlessly blends historic sanctuaries with ultra-modern landmarks, promising an unforgettable adventure in your next vacation. Use our hand-picked five-day schedule to make every minute count.
[h2]Kick-off – Classic Meets Cutting-Edge[/h2]
Begin at Senso-ji Temple, meander Nakamise Street for local snacks, then breathe in Ueno Park. Cap the evening atop the soaring Skytree for panoramic views.
[h2]Foodie Quest – Markets to Trendy Streets[/h2]
Rise early at bustling Tsukiji to sample street snacks. Head next to youthful Harajuku lanes for kawaii culture.
[h2]Day 3 – Museums to Ginza[/h2]
Immerse yourself in world-class galleries, then treat yourself in glitzy Ginza. Finish with Roppongi art spaces for a aesthetic finale.
[h2]Fourth Day – Royal Gardens & Tokyo Tower[/h2]
Wander the moat-lined palace paths, snap photos at stone bridges, then ascend the 333 m tower for breathtaking cityscapes.
[h2]Day 5 – Onsen, Tea & Yanaka[/h2]
Conclude with an indoor hot spring in bayside Odaiba, enjoy a matcha experience, and browse Yanaka’s craft shops before you head home.
[align=center]Ready to plan? Head [url=https://itimaker.com/blog/tokyo-itinerary]the article to craft your dream Tokyo adventure![/align]
Клининг в Москве становится все более популярным. Благодаря высоким темпам жизни жители мегаполиса ищут способы упростить быт.
Услуги клининговых компаний включают в себя множество различных задач. Профессиональный клининг включает как стандартную уборку, так и глубокую очистку в зависимости от потребностей клиентов.
При выборе клининговой компании важно обратить внимание на опыт работы и отзывы клиентов. Клиенты должны понимать, что качественная уборка требует профессиональных навыков и соблюдения стандартов.
Таким образом, услуги клининга в Москве предоставляют возможность сэкономить время. Клиенты могут легко найти компанию, предоставляющую услуги клининга, для поддержания чистоты.
клининговые услуги в москве [url=http://www.uborkaklining1.ru]http://www.uborkaklining1.ru[/url] .
сколько стоит керамогранитная плитка [url=http://kermogranit-kupit.ru]http://kermogranit-kupit.ru[/url] .
керамогранит недорого москва [url=kermogranit-kupit1.ru]керамогранит недорого москва[/url] .
dj онлайн [url=http://klubnaya-muzyka33.ru]dj онлайн[/url] .
сколько стоит керамогранит 60 на 60 [url=kermogranit-kupit1.ru]kermogranit-kupit1.ru[/url] .
керамогранит напольный москва [url=kermogranit-kupit.ru]kermogranit-kupit.ru[/url] .
самые лучшие клубные треки [url=https://klubnaya-muzyka33.ru]самые лучшие клубные треки[/url] .
301 Moved Permanently [url=https://zooaquarium.ru]301 Moved Permanently…[/url]
Посетите наш сайт и узнайте о [url=https://uborka-chistota.ru/]сколько стоят услуги клининговой компании[/url]!
Клининговые услуги в Санкт-Петербурге набирают популярность. С каждым годом увеличивается количество компаний, предоставляющих разнообразные услуги по уборке.
Заказчики высоко оценивают качество и доступность клининговых услуг. Многие клининговые фирмы предлагают персонализированные решения для каждого клиента, принимая во внимание его желания.
В спектр клининговых услуг входят как плановые уборки, так и одноразовые мероприятия
[url=https://bitqt-official.com/]Bitqt app[/url] skraca czas reakcji na zmiany na rynku dzięki alertom i automatyzacji. Handel w aplikacji jest bezpieczny i przejrzysty.
Bitqt to nowoczesna platforma do handlu, która umożliwia inwestorom handel na rynkach finansowych. Dzięki zaawansowanym algorytmom, Bitqt analizuje rynki w czasie rzeczywistym, co pozwala użytkownikom podejmować świadome decyzje inwestycyjne.
Platforma oferuje szereg narzędzi, które ułatwiają trading. Użytkownicy mają możliwość skorzystania z automatyzacji handlu, co zwiększa potencjalne zyski. Interfejs systemu jest łatwy w obsłudze, co czyni go dostępnym dla początkujących inwestorów.
Bezpieczeństwo użytkowników jest priorytetem dla Bitqt. Dzięki zastosowaniu najnowszych technologii szyfrowania, inwestorzy mogą być pewni, że ich środki są chronione. To sprawia, że Bitqt jest zaufanym wyborem dla wielu inwestorów.
Reasumując, Bitqt stanowi doskonałą opcję dla inwestorów pragnących handlować na rynkach. Dzięki innowacyjnym funkcjom, bezpieczeństwu oraz intuicyjnej obsłudze, każdy może rozpocząć swoją inwestycyjną przygodę. Zainwestuj w przyszłość z Bitqt.
Закажите [url=https://uborka12.ru/]клининг СПб[/url] на удобное время — мы приедем вовремя и выполним всё по договору. Довольны останетесь и вы, и ваш интерьер.
Клининг в Санкт-Петербурге становится всё более популярным. Существует множество фирм, предоставляющих разнообразные клининговые услуги. Клининговые компании предлагают уборку жилых и коммерческих объектов.
Многие люди предпочитают услуги клининга для того, чтобы сэкономить время. Это позволяет им уделять время другим аспектам жизни. Услуги клининга идеально подходят для тех, кто ведет активный образ жизни.
Одна из основных причин популярности клининговых компаний – это профессионализм. Специалисты обучены использовать современное оборудование и эффективные моющие средства. Такой подход позволяет быстро и качественно выполнять работу.
Разнообразие пакетов услуг позволяет каждому найти подходящее решение. Некоторые клининговые фирмы предоставляют услуги по разовой уборке, тогда как другие предлагают долгосрочные контракты. Так клиенты могут подобрать наиболее удобный для себя вариант.
Интенсивное [url=https://kursi-barbera-s-nulya.ru/]барбершоп обучение мастеров[/url] включает всё — от fade до классики. Индивидуальный подход и поддержка.
Все больше людей интересуются курсами барбера. Учебные заведения все чаще предлагают курсы для барберов. Рост популярности мужских стрижек и ухаживающих процедур объясняет интерес к таким курсам.
На таких курсах обучают не только основам стрижки, но и искусству общения с клиентами. Студенты обучаются всем необходимым навыкам для успешного старта в профессии. Они изучают различные стили и техники стрижки, а также уход за волосами и бородой.
По завершению обучения, всем выпускникам предоставляется шанс найти работу в салонах или открыть свою барберскую студию. Месторасположение и репутация учебного заведения также играют важную роль в выборе курсов. Важно изучить отзывы и рекомендации перед тем, как записываться на курсы.
Выбор подходящих курсов барбера должен основываться на ваших целях и ожиданиях. С каждым днем рынок барберинга расширяется, поэтому качество образования становится решающим. Необходимо учитывать, что достижения в этой профессии требуют непрерывного образования и практического опыта.
Всё, как вы любите — [url=https://sakura-v-spb.ru/]доставка суши СПб[/url] с высоким уровнем сервиса и точной логистикой.
Заказ вок-блюд через интернет приобретает все большую популярность. Существует множество причин, почему вок-заказ стал любимым среди людей.
Вок-блюда можно заказать в больших и малых ресторанах, которые специализируются на этой кухне. Каждый ресторан имеет свои особенности и уникальные блюда в меню.
Чтобы сделать правильный выбор, стоит обратить внимание на отзывы. Это позволит выбрать только те рестораны, которые предлагают отличное качество пищи.
Иногда рестораны предлагают привлекательные скидки на вок-блюда, что делает заказ еще более приятным. Акции могут значительно снизить общую стоимость заказа, что радует клиентов.
The magic of [url=https://drone1-show.com/]light drones[/url] turns any celebration into a spectacle of light, movement, and unforgettable moments.
In recent years, drone light shows have gained significant popularity. These spectacular displays use coordinated drones to create stunning visual effects. They serve as a contemporary substitute for conventional fireworks. A lot of event organizers are integrating this novel technology.
One significant advantage of drone light shows is that they are environmentally friendly. In contrast to fireworks, they do not generate detrimental smoke or waste. This makes them a safer option for public events. Moreover, they can be customized to fit various themes and occasions.
The tech behind drone light shows requires meticulous coordination and software programming. These drones are fitted with lights that can alter hues and designs. This advanced technology facilitates engaging displays that can enthrall spectators. In essence, drone light shows represent the future of entertainment.
Looking ahead, the possibilities for drone light shows are immense. With technological progress, we can anticipate increasingly complex and spectacular performances. These events will not only entertain but also leave a lasting impression on audiences. The entertainment landscape is certainly brightened by the emergence of drone light shows.
Con nuestro [url=https://show1-de-drones.com/]espectaculo drones[/url], tu evento brillará como nunca antes. Desde animaciones flotantes hasta logotipos en el cielo, adaptamos cada show para impactar visual y emocionalmente a la audiencia.
La popularidad de los espectáculos de drones ha crecido exponencialmente en los últimos tiempos. Estos eventos combinan tecnología, arte y entretenimiento. Las exhibiciones de drones son cada vez más comunes en festivales y celebraciones.
Los drones equipados con luces generan figuras fascinantes en el firmamento. Los asistentes se sorprenden con la sincronización y el despliegue de luces en el aire.
Varios organizadores deciden recurrir a compañías dedicadas a la producción de espectáculos de drones. Dichas compañías tienen personal cualificado y los equipos más modernos disponibles.
La seguridad representa un factor fundamental en la realización de estos eventos. Se siguen procedimientos detallados para prevenir riesgos durante estas exhibiciones. El futuro de los espectáculos de drones es prometedor, con innovaciones constantes.
Favori yapımlarınızı [url=https://trfullhdizle.com/]full film izle 4k[/url] konforuyla takip edin. Yüksek çözünürlükle evde sinema keyfini dorukta yaşayın.
büyüyen bir trend haline geldi. Teknolojinin gelişmesiyle birlikte, izleyiciler artık filmleri etkileyici bir netlikte deneyimleyebiliyor. 4K filmlerin keskinliği ve detayları izleme deneyimini bambaşka bir seviyeye taşıyor.
Çeşitli platformlar 4K’da Full HD film izleme olanağı sunuyor. Bu servisler film kalitesini geliştirerek izleme zevkini artırıyor. Netflix ve Amazon Prime gibi önde gelen servisler geniş bir 4K içerik arşivine sahip. Bu geniş koleksiyon farklı zevklere ve tercihlere hitap ediyor.
Bu deneyimi tam anlamıyla yaşamak için uygun bir cihaz gereklidir. Çoğu modern televizyon ve projeksiyon cihazı 4K’yı desteklemektedir. Donanımınızın özelliklerini kontrol ederek 4K oynatmaya uygun olduğundan emin olun.
Nihayetinde, 4K’da Full HD film izleme deneyimi rakipsizdir. Doğru araçlar ve sağlam yayın servisleriyle büyüleyici görselleri keşfetmeniz mümkün. Bu fırsatı kaçırmayın ve film keyfinizi yeni bir seviyeye taşıyın.
Göz kamaştırıcı netlikte izleme deneyimi için [url=https://turkfilmsitesi.com/]hd film izle türkçe dublaj[/url] arşivine göz atın. Gerçek kalite şimdi çok yakın.
Full HD bir filmi deneyimlemek gerçekten büyüleyicidir. Teknolojinin evrimi, film kalitesini önemli ölçüde iyileştirdi. Günümüzde izleyiciler, nefes kesici görselleri ve etkileyici sesleri birlikte deneyimleyebiliyor.
Son yıllarda 4K çözünürlüğe olan ilgi önemli ölçüde arttı. 4K, standart HD’ye göre daha keskin ve detaylı görüntüler sağlar. Birçok film tutkunu için 4K formatında film izlemek vazgeçilmezdir.
Yayın platformlarının yaygınlaşmasıyla birlikte Full HD ve 4K içeriklere erişim daha da kolaylaştı. İzleyiciler sevdikleri filmleri her an ve her yerden izleme imkanına sahip. Bu kolaylık, medya tüketim şeklimizi kökten değiştirdi.
4K içeriklerin artmasıyla birlikte yüksek kaliteli ekranlara olan talep de artıyor. Kaliteli bir 4K televizyona yatırım yapmak izleme deneyimini önemli ölçüde iyileştirir. Gerçek film tutkunları için bu yatırım kesinlikle buna değer.
Full HD Türkçe dublaj kategorimiz, kaliteli ve sevilen filmlerle doludur. Kesintisiz izleme için [url=https://trfilmcehennemi.com/]full hd türkçe dublaj[/url] sayfasını kullanabilirsiniz.
Son yıllarda yayın platformlarının yükselişi dikkat çekici oldu. Yüksek kaliteli içerikler, özellikle Full HD ve 4K filmler, izleyicilerin büyük ilgisini çekiyor. İnsanlar, netlik ve detaylara vurgu yapan etkileyici izleme deneyimleri arayışında.
Full HD filmler 1920×1080 piksel çözünürlük sunarak etkileyici görsel kalite sağlar. Bu, özellikle büyük ekranlarda her detayın fark edilebildiği durumlarda belirgindir. Buna karşılık, 4K filmler 3840×2160 piksel çözünürlükle izleme deneyimini olağanüstü hale getirir.
Yayın platformları bu trende kayıtsız kalmayarak şimdi geniş bir Full HD ve 4K film seçkisi sunuyor. Böylece, seyirciler hem yeni yapımları hem de sevilen klasik filmleri en yüksek görsel kalitede izleyebiliyor. Bunun yanında, birçok yayın hizmeti yüksek çözünürlüklü formatlara özel orijinal içerik üretimine kaynak ayırıyor.
Özetle, yayın hizmetlerinde Full HD ve 4K filmlere yönelim, izleyici tercihindeki değişimleri gösteriyor. Teknolojik gelişmelerle birlikte, izleme deneyimlerimizde daha yenilikçi çözümler görmemiz muhtemeldir. Bu gelişmeler kesinlikle sinema ve ev eğlencesinin geleceğini etkileyecektir.
Не ждите утра, закажите [url=https://vyvod-iz-zapoya-spb-01.ru/]вывод из запоя круглосуточно[/url] в СПб прямо сейчас. Наши специалисты готовы выехать для оказания неотложной наркологической помощи.
Процесс вывода из запоя является довольно трудным и требует особого внимания. Важно понимать, что каждая ситуация уникальна и требует индивидуального подхода.
Первым шагом в процессе вывода из запоя является решение обратиться к специалисту. Многие пытаются решить проблему самостоятельно, но это не всегда приводит к положительному результату.
Визит к врачу или наркологу — это ключевой момент при выводе из запоя. Врач сможет составить эффективный план лечения и назначить нужные лекарства.
Также очень важно иметь поддержку со стороны родных и друзей. Они могут оказаться важным источником силы и поддержки в это тяжелое время.
The Pokies Australia [url=http://thepokiesau.org]http://thepokiesau.org[/url] .
dragon slot [url=http://casinosdragonslots.eu/]http://casinosdragonslots.eu/[/url] .
the pokies net 250 [url=https://pokiesnet250.com/]https://pokiesnet250.com/[/url] .
The Pokies net Australia [url=thepokiesnet250.com]thepokiesnet250.com[/url] .
Комфорт и эффективность лечения в [url=https://narkologicheskaya-klinika01.ru/]частной наркологической клинике в Санкт-Петербурге[/url]. Индивидуальные программы и внимание к каждому пациенту.
Наркологическая клиника — это место, где люди могут получить профессиональную помощь в борьбе с зависимостями. Команда профессионалов в наркологической клинике обеспечивает индивидуальный подход к каждому пациенту.
Основной целью наркологической клиники является выявление и лечение проблем, связанных с зависимостями. Комплексный подход к лечению включает как медицинские, так и психологические методы.
Психологическая поддержка играет ключевую роль в процессе восстановления. Это помогает пациентам не только избавиться от физической зависимости, но и предотвратить рецидивы.
Каждый пациент проходит реабилитацию в своем темпе, что позволяет избежать стрессовых ситуаций. Однако, завоевание контроля над своей жизнью стоит затраченных усилий.
Большой выбор тщательно проработанных планировок ждет вас. Найдите свой идеальный вариант среди наших [url=https://proekty-domov1.ru/]готовых проектов домов и коттеджей[/url] и экономьте время на стадии проектирования.
Все больше людей обращают внимание на проекты домов при выборе жилья. Выбор подходящего проекта очень важен для создания комфортного дома.
На сегодняшний день предлагается разнообразие стилей и типов проектов домов. Каждый желающий может выбрать проект, отвечающий его личным предпочтениям.
При выборе проекта важно учитывать размеры участка. Анализировать климатические условия и окружение также следует при выборе проекта.
С использованием современных технологий возможно разработать индивидуальные проекты домов. Каждый проект может быть адаптирован под конкретные нужды заказчика.
Ищете комфортное и доступное по цене жилье в курортной Джубге? Наш сервис специализируется на подборе недорогих вариантов без потери качества. Найдите свой идеальный вариант для экономного отдыха [url=https://otdyh-v-dzhubge.ru/]джубга жилье недорого[/url].
Джубга предлагает уникальные возможности для летнего отдыха. Этот курорт славится своими пляжами и живописными пейзажами.
Множество туристов приезжает сюда каждый год, чтобы насладиться местными достопримечательностями. К числу популярных мест относятся водопады и древние дольмены.
Кроме того, Джубга предлагает разнообразные развлечения для всей семьи. Здесь можно заниматься различными видами активного отдыха, включая водные виды спорта и прогулки.
Отдых на пляже — это неотъемлемая часть вашего пребывания в Джубге. Пляжная жизнь в Джубге включает в себя купание, принятие солнечных ванн и дегустацию местной кухни в уютных кафе.
[url=https://cvetyvmoscve.ru/]Заказать цветы с доставкой в Москве[/url]
Доставка цветов в Москве – это удобный способ порадовать близких. Выбор сервисов по доставке цветов в Москве просто огромен, что позволяет найти идеальный вариант.
Перед тем как оформить заказ, необходимо определиться с тем, какие цветы вы хотели бы видеть в букете. Рекомендуется рассмотреть как стандартные варианты, так и более креативные решения.
Обратите внимание на сроки доставки и возможные дополнительные услуги. В некоторых компаниях вы можете добавить к своему заказу открытку или дополнительные небольшие презенты.
Выбирайте проверенные сервисы с хорошими отзывами и репутацией. Это гарантирует, что вы получите качественные цветы и обслуживание на высшем уровне.
Как сэкономить без потери комфорта? Советы по выбору жилья и времени заезда. Узнайте реальные [url=https://otdyh-v-arhipo-osipovke.ru/]отдых в архипо осиповке 2025 цены[/url] и оптимизируйте свои расходы.
Архипо-Осиповка — это удивительное место для отдыха. Отдых в этом курортном поселке привлекает туристов своим мягким климатом и великолепными видами.
Пляжи этого курорта известны своим чистым песком и спокойными водами. На пляжах Архипо-Осиповки доступны различные водные виды спорта и развлекательные программы.
Разнообразие мест для проживания в Архипо-Осиповке удовлетворит любые потребности отдыхающих. Гостиницы и частные номера в Архипо-Осиповке подойдут как для романтического уикенда, так и для семейного отдыха.
Здесь вы найдете множество развлечений для всей семьи. Вы сможете насладиться прогулками вдоль побережья, участвовать в экскурсиях и посещать местные мероприятия.
электрокарнизы [url=https://karniz-motorizovannyj77.ru/]электрокарнизы[/url] .
карнизы для штор с электроприводом [url=www.karnizy-s-elektroprivodom77.ru]карнизы для штор с электроприводом[/url] .
Для демонстрации видео высшего качества выберите специализированный [url=https://ehkrany-dlya-proektora1.ru/]экран для видеопроектора купить[/url] который можно в нашем магазине.
Экраны для проекторов играют значительную роль в успешной презентации контента. Правильный выбор экрана может существенно повлиять на восприятие информации.
Существует несколько типов экранов, таких как переносные, стационарные и на стену. Все эти типы экранов обладают определенными особенностями и могут удовлетворить разные потребности.
Выбирая экран, важно учитывать размер пространства и модель проектора. Оптимальные размеры экрана зависят от расстояния от него до зрителей.
Чтобы обеспечить лучшее восприятие картинки, нужно обращать внимание на уровень освещения. В условиях яркого света оптимальным решением станет экран с матовым фоном.
айфлоу [url=www.citadel-trade.ru]www.citadel-trade.ru[/url] .
электрокарнизы в москве [url=www.elektrokarniz90.ru]www.elektrokarniz90.ru[/url] .
готовые рулонные шторы цена [url=https://www.elektricheskie-rulonnye-shtory77.ru]https://www.elektricheskie-rulonnye-shtory77.ru[/url] .
рулонные жалюзи купить в москве [url=http://www.elektricheskie-rulonnye-shtory99.ru]рулонные жалюзи купить в москве[/url] .
рулонные шторы на пластиковые окна на кухню [url=https://rulonnye-shtory-s-elektroprivodom15.ru/]https://rulonnye-shtory-s-elektroprivodom15.ru/[/url] .
Хризантемные букеты с доставкой по Москве без дополнительных затрат — это отличное решение для всех, кто хочет порадовать близких. Хризантемы привлекают внимание своим многообразием и элегантностью. С помощью хризантем возможно формирование красивых цветочных ансамблей.
[url=https://hrizantemymsk.ru/]Букеты из хризантем с бесплатной доставкой по Москве[/url]
Мы предлагаем разнообразные варианты цветочных композиций. Каждый букет оформляется с особой тщательностью. Мы ценим уникальность вашего подарка, и наши букеты это подчеркивают.
Делая предзаказ, вы можете указать удобное время для доставки. Мы обеспечим доставку вашего букета своевременно и качественно. Каждый заказ доставляется нашими курьерами с максимальным вниманием и заботой.
Покупая букеты из хризантем, вы получаете не только красоту, но и радость. Подарите своим близким возможность насладиться ароматом и красотой хризантем. Мы готовы предложить вам лучшие варианты на любой случай жизни.
Узнайте точную стоимость проживания для планируемых дат. Мы предлагаем прозрачную [url=https://otdyhabhaziya01.ru/]отдых в абхазии цена[/url] без скрытых комиссий.
Абхазия — удивительное место для отдыха, полное красоты и уникальности. Её живописные пейзажи, мягкий климат и теплое море привлекают туристов со всего мира.
Многочисленные туристы выбирают Абхазию как идеальное место для отдыха и развлечений. На побережье Абхазии доступны различные виды активного отдыха и развлечений.
Каждый путешественник сможет найти подходящее место для проживания в Абхазии. Гастрономическая культура Абхазии порадует даже самых искушённых гурманов.
Отдых в Абхазии позволит вам забыть о повседневной рутине и насладиться моментом. Посетите Абхазию, и вы сможете насладиться её природными красотами и культурным наследием.
кашпо для дома напольное [url=https://kashpo-napolnoe-msk.ru/]кашпо для дома напольное[/url] .
sportbets [url=www.sportbets14.ru]www.sportbets14.ru[/url] .
Пригласите друзей на отдых в море и создайте настоящую атмосферу праздника — воспользуйтесь услугой [url=https://arenda-yahty-sochi07.ru/]яхты сочи аренда[/url] с возможностью выбора маршрута.
Прокат яхты — отличный вариант для тех, кто ищет новые приключения на воде. Путешествие на яхте позволяет насладиться красотой природы и расслабиться.
Правильный выбор яхты может значительно повлиять на ваше впечатление от отпуска. Тип и размер яхты имеют большое значение, поэтому выбирайте то, что подходит именно вам.
При аренде яхты важно внимательно изучить все пункты договора. Некоторые компании могут предлагать дополнительные услуги, такие как капитан или экипаж.
Наконец, не забудьте об организации маршрута. Проведите время в красивейших местах, которые доступны только с воды.
Букет гортензий с бесплатной доставкой в Москве — это отличное решение для тех, кто хочет удивить своих близких. Гортензии в букете символизируют любовь и дружбу, что делает их идеальными для подарка.
[url=https://gortenziimsk.ru/]Букет гортензий с бесплатной доставкой в Москве[/url].
Мы предлагаем доставку букета гортензий на самый удобный для вас адрес. Каждый букет гортензий создается мастерами флористики с любовью и вниманием.
Гортензии прекрасно дополняют любые цветочные композиции и подходят для различных случаев. Эти цветы могут стать стильным акцентом в вашем доме, радующим глаз каждый день.
Подарите себе или своим друзьям чудесный букет гортензий с доставкой на дом. Сделать заказ букета гортензий с доставкой очень просто и быстро.
Обновлённые предложения и гибкие условия бронирования делают [url=https://otdyhabhaziya0.ru/]абхазия отдых цены[/url] привлекательными для каждого туриста.
Абхазия — это удивительное место для отдыха. Пейзажи Абхазии поражают своей красотой и разнообразием.
Черноморское побережье Абхазии изобилует чудесными курортами. Гостевые дома и отели предлагают комфортные условия для проживания.
Уникальные природные чудеса Абхазии приятно удивляют отдыхающих. Горные пейзажи, живописные озера и величественные водопады манят туристов.
Любители вкусной еды найдут в Абхазии множество интересных блюд. Местная кухня славится своими свежими продуктами и яркими вкусами.
sportbets [url=http://sportbets17.ru/]http://sportbets17.ru/[/url] .
металлический значок на заказ [url=https://znacki-na-zakaz.ru/]znacki-na-zakaz.ru[/url] .
прогнозы на теннис го спорт [url=https://prognoz-na-segodnya-na-sport1.ru]https://prognoz-na-segodnya-na-sport1.ru[/url] .
прогнозы на баскетбол сегодня от профессионалов бесплатно [url=https://prognoz-na-segodnya-na-sport.ru/]https://prognoz-na-segodnya-na-sport.ru/[/url] .
sportbets [url=https://sportbets16.ru/]https://sportbets16.ru/[/url] .
ставки на сегодня футбол прогнозы точные [url=http://www.kompyuternye-prognozy-na-futbol1.ru]http://www.kompyuternye-prognozy-na-futbol1.ru[/url] .
Un [url=https://show1-de-drones.com/]show de luces con drones[/url] puede transformar cualquier entorno en una experiencia mágica y sensorial. Nuestro equipo diseña secuencias lumínicas que flotan en el aire con perfecta coordinación y belleza.
Los espectáculos de drones se han vuelto muy populares en la actualidad. Estos eventos combinan tecnología, arte y entretenimiento. Las demostraciones de drones son frecuentemente vistas en festivales y celebraciones importantes.
Los drones equipados con luces generan figuras fascinantes en el firmamento. Los asistentes se sorprenden con la sincronización y el despliegue de luces en el aire.
Muchos organizadores optan por contratar compañías especializadas para estos eventos. Estas organizaciones poseen pilotos entrenados y tecnología avanzada.
El tema de la seguridad es vital en la planificación de estos shows. Se implementan protocolos rigurosos para garantizar la protección de los asistentes. El futuro de los espectáculos de drones es prometedor, con innovaciones constantes.
спортивный прогноз на сегодня [url=http://www.prognoz-na-segodnya-na-sport3.ru]спортивный прогноз на сегодня[/url] .
прогнозы на спорт с анализом [url=http://kompyuternye-prognozy-na-futbol.ru]http://kompyuternye-prognozy-na-futbol.ru[/url] .
спортивный прогноз на сегодня [url=www.prognoz-na-segodnya-na-sport2.ru]www.prognoz-na-segodnya-na-sport2.ru[/url] .
супер прогнозы на спорт [url=http://www.kompyuternye-prognozy-na-futbol2.ru]http://www.kompyuternye-prognozy-na-futbol2.ru[/url] .
красивые напольные горшки для цветов [url=https://kashpo-napolnoe-spb.ru]https://kashpo-napolnoe-spb.ru[/url] .
прогнозы на форы в хоккее [url=https://luchshie-prognozy-na-khokkej1.ru/]luchshie-prognozy-na-khokkej1.ru[/url] .
интернет-магазин сантехники с доставкой по россии [url=https://www.internet-magazine-santehniki.ru]https://www.internet-magazine-santehniki.ru[/url] .
ставки на матч хоккей [url=https://www.luchshie-prognozy-na-khokkej.ru]https://www.luchshie-prognozy-na-khokkej.ru[/url] .
точный прогноз на спорт сегодня [url=https://kompyuternye-prognozy-na-futbol3.ru]точный прогноз на спорт сегодня[/url] .
прогноз на хоккей в прогнозе [url=luchshie-prognozy-na-khokkej2.ru]luchshie-prognozy-na-khokkej2.ru[/url] .
Descubre cómo un [url=https://show1-de-drones.com/]espectaculo de drones[/url] puede cambiar por completo la atmósfera de tu evento. Cientos de luces en el cielo se mueven al ritmo de la música, formando patrones, figuras y emociones inolvidables.
La popularidad de los espectáculos de drones ha crecido exponencialmente en los últimos tiempos. Estos shows integran tecnología avanzada, creatividad y diversión. Las presentaciones de drones se han convertido en una atracción habitual en festivales y acontecimientos.
Los drones equipados con luces generan figuras fascinantes en el firmamento. Los espectadores quedan maravillados con el espectáculo de luces y movimientos.
Numerosos planificadores de eventos eligen contratar a empresas expertas para llevar a cabo estos shows. Estas empresas cuentan con pilotos capacitados y equipos de última generación.
La seguridad representa un factor fundamental en la realización de estos eventos. Se siguen procedimientos detallados para prevenir riesgos durante estas exhibiciones. El porvenir de los espectáculos de drones es alentador, gracias a las constantes mejoras en la tecnología.
Ясность ума и продуктивность — ваш новый стандарт. [url=https://magazin-nootropov.ru/]Биохакер магазин ноотропов[/url] предлагает доступ к лучшим средствам без лишних усилий.
Ноотропы — это вещества, которые улучшают когнитивные функции человека. Ноотропы используются для стимуляции умственной активности, улучшения памяти и повышения уровня внимания.
Среди ноотропов можно выделить разнообразные препараты, включая как искусственные, так и натуральные. Все эти препараты различаются по своим механизму действия и конечным результатам.
Природные ноотропы, такие как женьшень и гинкго билоба, известны своими полезными свойствами. Данные природные ноотропы широко используются в лечебных целях для повышения внимательности и памяти.
Среди синтетических ноотропов, таких как пирацетам, выделяются препараты, обладающие специфическими действиями. Они часто применяются для лечения различных нарушений, включая проблемы с памятью.
ванная с гидромассажем купить [url=https://hidromassazhnaya-vanna.ru/]https://hidromassazhnaya-vanna.ru/[/url] .
gessi каталог [url=https://gessi-santehnika-1.ru]https://gessi-santehnika-1.ru[/url] .
услуги по согласованию перепланировки квартиры [url=https://soglasowanie-pereplanirovki-kvartiry.ru/]https://soglasowanie-pereplanirovki-kvartiry.ru/[/url] .
айфон 10 цена спб [url=https://kupit-ajfon-cs1.ru]https://kupit-ajfon-cs1.ru[/url] .
нужен проект перепланировки квартиры [url=www.proekt-pereplanirovki-kvartiry.ru]www.proekt-pereplanirovki-kvartiry.ru[/url] .
айфон центр [url=kupit-ajfon-cs.ru]kupit-ajfon-cs.ru[/url] .
где сделать проект перепланировки [url=https://proekt-pereplanirovki-kvartiry1.ru]https://proekt-pereplanirovki-kvartiry1.ru[/url] .
напольные горшки для цветов купить интернет [url=https://kashpo-napolnoe-rnd.ru/]напольные горшки для цветов купить интернет[/url] .
Dive into the world of colorful reels and thrilling spins with [url=https://sweet-bonanza25.com/]sweet bonanza[/url], where every moment could lead to a big win and exciting gameplay.
Sweet Bonanza is a popular online slot game that has captured the attention of players worldwide. This game features vibrant graphics and exciting gameplay, making it a favorite.
The primary attraction of Sweet Bonanza lies in its unique features. With its cascading reels, players can secure multiple victories on each spin.
On top of that, Sweet Bonanza provides a free spins option that enhances the overall fun. The potential for large payouts during free spins makes this aspect incredibly exciting.
To sum up, Sweet Bonanza is a captivating slot game that offers much to players. Its colorful aesthetics and lucrative features attract a wide range of players, from novices to veterans.
iphone spb [url=www.kupit-ajfon-cs2.ru]iphone spb[/url] .
mostbet mobil qeydiyyat [url=mostbet4049.ru]mostbet4049.ru[/url]
1win crash signal [url=www.1win3024.com]www.1win3024.com[/url]
1win withdrawal problem [url=1win3026.com]1win3026.com[/url]
Приобретайте только надежную технику для безопасной работы. Решили [url=https://gruzovoy-podjemnik15.ru/]купить подъемное оборудование[/url]? У нас лучший выбор и цены в Санкт-Петербурге.
Подъемное оборудование играет важную роль в современных строительных проектах. Оно используется для перемещения тяжелых грузов на высоту и облегчает рабочие процессы.
Разнообразие подъемного оборудования впечатляет: от подъемников до кранов и эскалаторов. Каждый тип подъемного оборудования находит свое применение в зависимости от специфики работы.
Перед использованием подъемного оборудования необходимо провести его технический осмотр. Регулярный технический осмотр помогает предотвратить поломки и обеспечивает безопасное использование оборудования.
Правила эксплуатации подъемного оборудования необходимо строго придерживаться для обеспечения безопасности. Только при соблюдении всех инструкций можно гарантировать успешное выполнение задач.
1win aviator login [url=https://www.1win3028.com]https://www.1win3028.com[/url]
купить apple спб [url=http://www.kupit-ajfon-cs3.ru]купить apple спб[/url] .
Незаменимый помощник для монтажных и отделочных работ на высоте. Безопасное использование [url=https://nozhnichnyy-podemniki15.ru/]ножничного подъемника в строительстве[/url] повысит эффективность вашей бригады.
Ножничный подъемник — это одно из самых популярных средств подъемной техники. Такой тип подъемника позволяет безопасно поднимать как людей, так и грузы на значительную высоту.
Основное преимущество ножничного подъемника заключается в его компактности и маневренности. Компактные размеры этого подъемника позволяют эффективно эксплуатировать его в небольших помещениях и на узких площадках.
Еще одним важным аспектом является возможность регулировки высоты поднятия. Возможность настройки высоты делает их универсальными для различных типов работ.
Ножничные подъемники часто используются в строительстве, на складах и в торговле. Эти подъемники являются важным инструментом, обеспечивающим безопасность и удобство работы на высоте.
Rental savings, for business and tourism.
one month car rental [url=neochorion.com /paphos-long-term-rental]neochorion.com /paphos-long-term-rental[/url] .
электрокарниз двухрядный цена [url=www.elektrokarniz5.ru/]www.elektrokarniz5.ru/[/url] .
Лучший выбор ламината в магазине напольных покрытий. [url=http://xn--1-7sba5anhi5b.xn--p1ai]http://xn--1-7sba5anhi5b.xn--p1ai[/url] .
ремонт телевизора toshiba [url=https://toshiba-servisnyj-centr.ru/]ремонт телевизоров тошиба в москве[/url] – профессиональный ремонт с гарантией качества.
электрокарнизы [url=elektrokarnizy-dlya-shtor1.ru]электрокарнизы[/url] .
перевод документов для визы на английский [url=www.trs-center.ru]www.trs-center.ru[/url] .
Пробковые покрытия купить в Москве недорого [url=https://probkovoe-pokritie1.ru/]probkovoe-pokritie1.ru[/url] .
Паркетная доска, покрытие для квартиры купить. [url=https://www.parketnay-doska2.ru]https://www.parketnay-doska2.ru[/url] .
mostbet az giriş [url=www.mostbet4048.ru]mostbet az giriş[/url]
1win tennis mərcləri [url=http://1win3037.com/]1win tennis mərcləri[/url]
Мы публикуем только актуальные и прозрачные данные. Если вас интересует [url=https://deti-eto-schastie.ru/]суррогатное материнство стоимость[/url], вы найдёте подробную информацию на платформе без скрытых условий.
Суррогатное материнство представляет собой уникальную возможность для пар, которые сталкиваются с трудностями зачатия. Эта практика становится все более популярной и востребованной в современном обществе.
Суррогатное материнство делится на два основных типа, каждый из которых имеет свои преимущества и недостатки. При традиционном типе суррогатного материнства суррогатная мама становится биологической матерью, так как используется ее яйцеклетка. В гестационном суррогатном материнстве суррогатная мать не имеет генетической связи с ребенком, так как эмбрион создается из клеток родителей.
Прежде чем обратиться к суррогатным матерям, следует взвесить все за и против данного шага. Необходимо учитывать финансовые, юридические и эмоциональные аспекты, которые могут возникнуть в процессе. Ключевым моментом является выбор агентства, которое предоставит всестороннюю помощь на этапе подготовки и реализации суррогатного материнства.
Суррогатное материнство затрагивает как медицинские, так и социальные аспекты, включая права и обязанности всех участников. Общественная поддержка и осведомленность о суррогатном материнстве помогают разрушить стереотипы и предвзятости. В итоге, суррогатное материнство предоставляет возможность стать родителями тем, кто не может иметь детей, если это происходит с соблюдением всех необходимых норм и правил.
Наш каталог помогает быстро подобрать мастера для любого события. В разделе [url=https://best-photographers-moscow.ru/]москва фотограф[/url] представлены профессионалы с проверенным опытом и отзывами.
Выдающиеся фотографы занимают особое место в мире визуального искусства. В этой публикации мы обсудим ряд выдающихся фотографов, чьи снимки оставляют неизгладимое впечатление.
Начнем с личности, которая высоко ценится в мире фотографии. Данный фотограф умеет ловить моменты, запечатлевая их во всей красе.
Еще одним замечательным представителем является фотограф, который специализируется на портретной съемке. Этот фотограф способен создать снимки, передающие характер и настроение модели.
В заключение стоит упомянуть мастера, который специализируется на съемке природы. Снимки этого фотографа поражают своей яркостью и детальной проработкой.
Купить инженерную доску [url=https://inzenernay-doska1.ru/]https://inzenernay-doska1.ru/[/url] .
масляный трансформатор [url=https://www.fanfiction.borda.ru/?1-9-0-00001185-000-0-0-1752134950]масляный трансформатор[/url] .
где заказать проект перепланировки квартиры в москве [url=http://mymoscow.forum24.ru/?1-6-0-00030606-000-0-0-1751610212/]где заказать проект перепланировки квартиры в москве[/url] .
1win kazinosu [url=https://1win3041.com/]https://1win3041.com/[/url]
аппарат для узи купить [url=https://kupit-uzi-apparat8.ru/]https://kupit-uzi-apparat8.ru/[/url] .
1win android yukle [url=www.1win3040.com]www.1win3040.com[/url]
[url=byfurniture.ry]Дизайнерская мебель премиум класса[/url] — это воплощение изысканного стиля и безукоризненного качества.
Инвестиции в премиум мебель оправданы, так как она может служить долгие годы.
металлические сваи винтовые для фундамента [url=https://ostankino-svai.ru /]https://ostankino-svai.ru /[/url] .
Need to test services or register without giving your own number? Try our [url=https://receive-sms-online-fast.com/]temp sms[/url] solution for fast, simple, and private SMS reception.
Receiving SMS messages is an essential part of modern communication. These messages keep us in touch with our friends, family, and workmates.
With the rise of technology, SMS has turned into a key communication tool for numerous individuals. From reminders to updates, SMS serves a variety of purposes.
Nonetheless, certain individuals encounter difficulties when receiving SMS. Factors like connectivity issues, device settings, or technical malfunctions can lead to SMS delivery challenges.
Users can troubleshoot these issues by ensuring their network is active and their phone configurations are correct. Keeping the device’s software up to date may enhance SMS performance.
мед аппарат узи [url=https://www.kupit-uzi-apparat9.ru]https://www.kupit-uzi-apparat9.ru[/url] .
Хотите подчеркнуть свою индивидуальность? Тогда [url=https://pechat-na-futbolkah0.ru/]заказать футболку со своим принтом[/url] — это идеальное решение. Удобно, просто и без лишней волокиты.
Печать на футболках — это отличный способ выразить свою индивидуальность. Технологии печати открывают широкие горизонты для дизайнеров и любителей моды.
Методы печати на текстиле различаются по своим характеристикам и подходам. Например, трафаретная печать известна своей долговечностью и яркостью красок. Однако цифровая печать предоставляет больше возможностей для сложных дизайнов.
Важно помнить, что выбор ткани влияет на качество печати и долговечность изделия. Некоторые ткани лучше подходят для трафаретной печати, в то время как другие — для цифровой.
Количество заказываемых футболок может существенно изменить ваши затраты на печать. Для массового производства чаще используется трафаретная печать, а для небольших заказов — цифровая.
Хотите быстро въехать в уютное жилье? Выберите [url=https://karkasnye-doma0.ru/]каркасный дом под ключ[/url] — это удобный и экономичный способ строительства с гарантией качества.
В последнее время каркасные дома привлекают всё больше внимания среди людей, желающих построить жильё. Эти конструкции предлагают множество преимуществ, включая быстроту возведения и хорошую теплоизоляцию.
Одним из главных плюсов каркасного дома является его экономичность. Строительство каркасного дома снижает общие затраты как на материалы, так и на трудозатраты.
Кроме того, каркасные дома легко адаптируются под различные климатические условия. С их помощью можно строить комфортное жильё для проживания в любых климатических зонах.
Однако, стоит также учитывать недостатки каркасных домов. Например, по сравнению с кирпичными домами, каркасные имеют меньшую огнестойкость. Эти аспекты важно принимать во внимание при выборе типа дома.
тмг цены [url=www.maslyanie-transformatory-kupit.ru]www.maslyanie-transformatory-kupit.ru[/url] .
узи сканер купить москва [url=http://kupit-uzi-apparat15.ru]http://kupit-uzi-apparat15.ru[/url] .
цена узи аппарата [url=https://kupit-uzi-apparat10.ru/]kupit-uzi-apparat10.ru[/url] .
balloon 1win [url=1win3044.com]1win3044.com[/url]
трансформаторы масляные [url=https://maslyanie-transformatory-kupit2.ru]трансформаторы масляные[/url] .
масляные трансформаторы [url=https://maslyanie-transformatory-kupit1.ru/]maslyanie-transformatory-kupit1.ru[/url] .
пластиковые окна в москве [url=http://1okno-krasnodar.ru/]пластиковые окна в москве[/url] .
1win lucky jet [url=http://1win3048.com]1win lucky jet[/url]
Выбирая нас, вы получаете [url=https://derevyannye-doma-pod-klyuch97.ru/]деревянные дома под ключ[/url], в которых сочетаются натуральные материалы, современный дизайн и профессиональный подход.
В последнее время деревянные дома под ключ привлекают внимание людей, стремящихся к уютному загородному отдыху. Деревянные дома очаровывают своим естественным видом и экологическими свойствами.
Главное преимущество деревянных домов заключается в быстроте их строительства. Современные технологии позволяют возводить такие здания в кратчайшие сроки.
Деревянные дома также отличаются высокой теплоизоляцией. Зимой в них тепло, а летом они остаются прохладными.
Уход за деревянными домами довольно прост и не требует больших усилий. Частая обработка дерева специальными средствами способствует увеличению срока службы конструкции.
техническая вода цена [url=http://dostavka-tehnicheskoi-vodi.ru/]http://dostavka-tehnicheskoi-vodi.ru/[/url] .
прогнозы и ставки на спорт [url=http://stavki-na-sport-prognozy.ru/]http://stavki-na-sport-prognozy.ru/[/url] .
Повышайте качество оптимизации и учитесь работать с алгоритмами поисковых систем на [url=https://seoflagman.ru/]курсы по seo оптимизации[/url], ориентированных на современные тренды и методы.
Рост популярности курсов по SEO заметен среди новых владельцев бизнеса. Участники курсов получают знания о том, как правильно оптимизировать сайты для появления в топах поисковиков.
Первый шаг к успешному продвижению — изучение основ SEO. В курсе затрагиваются аспекты, связанные с выбором ключевых фраз, созданием качественного контента и построением ссылок.
Участие в практических заданиях помогает закрепить теоретические сведения. Участники курсов работают с реальными проектами, что помогает им лучше подготовиться к будущей работе.
Сертификаты, выдаваемые по завершении обучения, могут стать хорошим дополнением к резюме. Эти сертификаты могут стать важным фактором при трудоустройстве в сфере интернет-маркетинга.
Строительство начинается с идеи. На сайте вы найдёте [url=https://proekty-domov0.ru/]готовые проекты дома[/url], которые позволят вам сразу перейти к реализации без задержек и лишних затрат.
Проекты домов играют значимую роль для людей, задумывающихся о строительстве. Разработка качественного и функционального проекта может значительно упростить процесс строительства.
Начальным шагом в создании проекта является определение стиля и типа строения. Важно учесть не только личные предпочтения, но и особенности участка, на котором будет располагаться дом.
Следующий шаг — это планировка внутренних помещений. Необходимо понять, как будут взаимодействовать разные комнаты и учесть их функциональность.
Кроме того, необходимо задуматься о том, какие материалы и технологии будут использоваться при строительстве. Выбор материалов имеет огромное значение для долговечности и качества дома.
Ознакомьтесь с предложениями — [url=https://karkasnye-doma0.ru/]каркасные дома цены[/url] указаны за комплектацию под ключ. Выберите подходящий проект с гарантией.
Каркасные дома набирают популярность среди застройщиков. Такие дома имеют ряд преимуществ, таких как скорость строительства и высокая энергоэффективность.
Основным преимуществом каркасных конструкций является их доступная цена. Строительство такого дома позволяет значительно сократить затраты на материалы и рабочую силу.
Кроме того, каркасные дома легко адаптируются под различные климатические условия. С их помощью можно строить комфортное жильё для проживания в любых климатических зонах.
Однако, стоит также учитывать недостатки каркасных домов. Например, по сравнению с кирпичными домами, каркасные имеют меньшую огнестойкость. Эти аспекты важно принимать во внимание при выборе типа дома.
сайт ставков [url=www.stavki-na-sport-prognozy2.ru/]www.stavki-na-sport-prognozy2.ru/[/url] .
прогноз ставки [url=https://stavki-na-sport-prognozy1.ru/]https://stavki-na-sport-prognozy1.ru/[/url] .
прогнозы на ставки на спорт на сегодня [url=https://prognozy-na-sport-2.ru/]https://prognozy-na-sport-2.ru/[/url] .
футбол прогнозы [url=https://prognozy-na-futbol-1.ru/]https://prognozy-na-futbol-1.ru/[/url] .
точные прогнозы на спорт от профессионалов [url=www.prognozy-na-sport-3.ru/]www.prognozy-na-sport-3.ru/[/url] .
футбол сегодня прогнозы [url=https://prognozy-na-futbol-2.ru/]https://prognozy-na-futbol-2.ru/[/url] .
бесплатный прогноз на спорт [url=https://prognozy-na-sport-1.ru/]prognozy-na-sport-1.ru[/url] .
прогноз на сегодняшний хоккей [url=http://prognozy-na-khokkej-segodnya.ru]http://prognozy-na-khokkej-segodnya.ru[/url] .
прогноз на хоккей сегодня от профессионалов бесплатно [url=www.prognozy-na-khokkej-segodnya1.ru]www.prognozy-na-khokkej-segodnya1.ru[/url] .
Гидроизоляция зданий https://gidrokva.ru и сооружений любой сложности. Фундаменты, подвалы, крыши, стены, инженерные конструкции.
Эстетика, энергоэффективность и практичность — всё это предлагают [url=https://karkasnye-doma-vspb0.ru/]каркасные дома санкт петербург[/url], доступные на заказ по фиксированной цене с учетом пожеланий заказчика.
Строительство каркасного дома стало весьма распространенным в последние годы. Такие дома обладают рядом достоинств, включая быстрый монтаж и отличные теплоизоляционные свойства.
При строительстве каркасного дома важно учитывать качество используемых материалов. Необходимо уделять внимание таким материалам, как утеплитель и отделка, чтобы обеспечить надежность конструкции.
При выборе каркасного дома необходимо внимательно изучить проект и размеры будущего здания. Хорошо продуманный проект обеспечит удобное и функциональное использование пространства.
В конечном счете, каркасный дом будет хорошим выбором для создания уютного и теплого жилища. Также, его строительство не требует существенных временных и материальных ресурсов.
Упростите управление активами — [url=https://lizing-auto-top77.ru/]лизинг коммерческих автомобилей[/url] снижает финансовую нагрузку и позволяет гибко распоряжаться техникой.
Лизинг автомобилей для коммерческих нужд является выгодным решением для компаний. С его помощью можно быстро обновить автопарк, не прибегая к большим расходам.
Важно отметить, что лизинговые компании часто предлагают выгодные условия по обслуживанию. Таким образом, предприниматели могут сконцентрироваться на развитии бизнеса, не беспокоясь о состоянии автомобилей.
Выбор подходящих условий лизинга — важный этап для бизнеса. Разные лизинговые компании предоставляют возможность выбора сроков договора и размеров ежемесячных взносов.
Важно также учитывать налоговые преимущества лизинга. Компаниям доступна возможность вычета затрат на лизинг из налогооблагаемой базы.
швейцарские часы онлайн оценка [url=http://ocenka-chasov-onlajn8.ru]http://ocenka-chasov-onlajn8.ru[/url] .
оценка наручных часов [url=https://ocenka-chasov-onlajn9.ru/]оценка наручных часов[/url] .
Новые [url=https://apple-tula1.ru/]AirPods[/url] обеспечивают великолепное качество звука и удобство эксплуатации, делая прослушивание музыки и звонки максимально комфортными в любых условиях.
Apple является одним из самых известных и уважаемых брендов в мире технологий. Apple выпускает разнообразные товары, начиная от iPhone и заканчивая iPad и Mac.
Одним из ключевых факторов успеха Apple является инновационный дизайн. Компания постоянно стремится к улучшению пользовательского опыта и функциональности своих устройств.
Экосистема Apple предоставляет пользователям уникальные возможности для взаимодействия. Продукция Apple обладает высокой степенью совместимости, что делает их использование более удобным.
Несмотря на свою цену, устройства Apple остаются в большом спросе на рынке. Клиенты ценят надежность, высокое качество и передовые технологии, которые предоставляет Apple.
Легкость монтажа и надёжность гарантируют [url=https://metall-tula1.ru/]труба профильная[/url], востребованная в различных сферах строительства и производства.
Металлопрокат является основой для многих промышленных процессов. Сфера применения металлопроката включает строительство, автомобилестроение и много других областей. Существуют разнообразные виды металлопроката, которые подходят для разных задач.
К основным видам металлопроката относятся алюминий, сталь и другие металлические сплавы. Каждый из этих типов имеет свои особенности и преимущества. Например, сталь отличается высокой прочностью, а алюминий — легкостью и коррозионной стойкостью.
Металлопрокат также делится по способу обработки. Существует горячекатаный, холоднокатаный и профилированный металлопрокат. Определение способа обработки зависит от предполагаемых условий использования и требований к материалу.
При выборе металлопроката следует внимательно относиться к качеству, типу и репутации поставщика. Качество выбираемого металлопроката имеет решающее значение для прочности и надежности конечного продукта. Рекомендуется сотрудничать только с надежными производителями и тщательно проверять все сертификаты.
Для тех, кто ищет практичный и надежный вариант загородного жилья, [url=https://karkasnye-doma-vspb0.ru/]каркасный дом под ключ спб[/url] — отличный выбор. Строим по современным стандартам и адаптируем проекты под клиентов.
Каркасный дом — это один из самых популярных типов жилья в современном строительстве. Они предлагают множество преимуществ, таких как быстрая сборка и высокая теплоизоляция.
Качество стройматериалов — ключевой фактор при возведении каркасного дома. Необходимо уделять внимание таким материалам, как утеплитель и отделка, чтобы обеспечить надежность конструкции.
При выборе каркасного дома следует обращать внимание на проект и размеры. Правильное планирование позволит организовать пространство функционально и удобно.
В итоге, каркасный дом может стать идеальным вариантом для вашего будущего жилья. Кроме того, возведение такого дома не требует больших временных и финансовых затрат.
оценка часов в москве бесплатно [url=https://ocenka-chasov-onlajn10.ru/]https://ocenka-chasov-onlajn10.ru/[/url] .
доставка воды на дачу [url=http://dostavka-tehnicheskoi-vodi.ru]http://dostavka-tehnicheskoi-vodi.ru[/url] .
лестницы заказать [url=http://www.lestnicy-na-metallokarkase-1.ru]http://www.lestnicy-na-metallokarkase-1.ru[/url] .
изготовление и монтаж лестниц [url=https://lestnicy-na-metallokarkase-2.ru]https://lestnicy-na-metallokarkase-2.ru[/url] .
изготовление лестниц для загородного дома [url=https://lestnicy-na-metallokarkase-4.ru]изготовление лестниц для загородного дома[/url] .
Заказать диплом https://diplomikon.ru быстро, надёжно, с гарантией! Напишем работу с нуля по вашим требованиям. Уникальность от 80%, оформление по ГОСТу.
Оформим реферат https://ref-na-zakaz.ru за 1 день! Напишем с нуля по вашим требованиям. Уникальность, грамотность, точное соответствие методичке.
Отчёты по практике https://gotov-otchet.ru на заказ и в готовом виде. Производственная, преддипломная, учебная.
Диплом под ключ https://diplomnazakaz-online.ru от выбора темы до презентации. Профессиональные авторы, оформление по ГОСТ, высокая уникальность.
https://dibujando.net/comment/520766#comment-520766
купить лестницу на заказ [url=https://lestnicy-na-metallokarkase-3.ru/]https://lestnicy-na-metallokarkase-3.ru/[/url] .
Услуги по профессиональной уборке любого уровня сложности. [url=https://kliningovaya-kompaniya-v-spb-01.ru/]клининговые услуги в санкт петербурге[/url] — это надежный способ поддерживать порядок без лишних забот.
Клининг в Санкт-Петербурге – это важная услуга для множества людей и бизнесов. Чистота и порядок имеют большое значение в рабочей среде. Многие компании предлагают клининговые услуги.
При выборе клининговой компании важно понимать ваши требования. Необходимо выяснить, требуется ли уборка жилых помещений или коммерческих пространств. Также важно учитывать частоту уборки.
Следующий шаг – выбрать надежную клининговую фирму. Обратите внимание на отзывы клиентов. Надежные компании предоставляют гарантии на свои услуги.
Наконец, прежде чем сделать выбор, обязательно сравните цены. Цены на клининговые услуги могут различаться в зависимости от фирмы. Не всегда высокая цена означает лучшее качество.
https://www.alkoholik.cz/zavislost/forum/7-snazim-se-abstinovat/66784-rozhodl-jsem-se-jet.html#66784
Оперативная поставка и профессиональный монтаж в городе на Неве. Выбирайте проверенный [url=https://gruzovoy-podjemnik15.ru/]грузовой подъемник спб[/url] для вашего предприятия.
Современные строительные проекты не обходятся без подъемного оборудования. Подъемное оборудование существенно упрощает задачу по перемещению больших грузов на значительные высоты.
Подъемное оборудование делится на несколько категорий, таких как подъемники, краны и прочие механизмы. Выбор типа подъемного оборудования зависит от задач и условий эксплуатации, что делает его разнообразным.
Перед эксплуатацией подъемного оборудования крайне важно провести его тщательный технический осмотр. Проверка состояния техники позволяет избежать аварийных ситуаций и обеспечить безопасность.
Правила эксплуатации подъемного оборудования необходимо строго придерживаться для обеспечения безопасности. Только при соблюдении всех инструкций можно гарантировать успешное выполнение задач.
Уникальное сочетание комфорта, свежего морского воздуха и расслабляющей атмосферы подарит [url=https://morskie-progulki-1sochi.ru/]морская прогулка сочи[/url] — идеальный вариант для романтики или отдыха с друзьями.
Морские прогулки в Сочи – это уникальный способ провести время у моря. Каждый год тысячи туристов выбирают этот курорт для создания незабываемых воспоминаний.
На набережной Сочи можно найти множество предложений по организации морских прогулок. Гости курорта могут наслаждаться как короткими, так и длительными прогулками вдоль живописного побережья.
Прогулки по морю дарят возможность увидеть великолепные пейзажи Черного моря и гор. Многие маршруты включают наблюдение за дельфинами и другими морскими существами.
Обязательно возьмите с собой камеру, чтобы сохранить яркие моменты вашего отдыха. Морские прогулки в Сочи – это отличный способ провести время с друзьями и семьей.
ai therapist [url=https://ai-therapist23.com/]ai therapist[/url] .
ai therapy [url=https://ai-therapist24.com/]ai therapy[/url] .
esim switzerland sim united states
Когда все другие способы уже испробованы, наступает момент принять важное решение. На платформе вы найдёте надёжные профили, если [url=https://deti-eto-schastie.ru/]ищу суррогатную маму[/url] — это ваш актуальный запрос.
Суррогатное материнство открывает двери для семей, мечтающих о детях, но не способных их родить. Увеличение интереса к суррогатному материнству объясняется изменением общественного мнения и ростом технологий в области репродукции.
Суррогатное материнство делится на два основных типа, каждый из которых имеет свои преимущества и недостатки. При традиционном суррогатном материнстве яйцеклетка суррогатной матери оплодотворяется сперматозоидом партнера или донора. В отличие от этого, при гестационном суррогатном материнстве эмбрион создается с использованием яйцеклетки и сперматозоидов намеревающихся родителей.
Прежде чем обратиться к суррогатным матерям, следует взвесить все за и против данного шага. Необходимо учитывать финансовые, юридические и эмоциональные аспекты, которые могут возникнуть в процессе. Выбор подходящего агентства, которое будет сопровождать на каждом этапе, играет ключевую роль в успешном завершении процесса.
Суррогатное материнство затрагивает как медицинские, так и социальные аспекты, включая права и обязанности всех участников. Общественная поддержка и осведомленность о суррогатном материнстве помогают разрушить стереотипы и предвзятости. В итоге, суррогатное материнство предоставляет возможность стать родителями тем, кто не может иметь детей, если это происходит с соблюдением всех необходимых норм и правил.
Чтобы результат съёмки радовал долгие годы, выбирайте профессионала. Здесь вы легко найдёте [url=https://best-photographers-moscow.ru/]лучший фотограф[/url] с высоким рейтингом и подтверждёнными отзывами.
Выдающиеся фотографы занимают особое место в мире визуального искусства. В этой публикации мы обсудим ряд выдающихся фотографов, чьи снимки оставляют неизгладимое впечатление.
Первым стоит выделить имя, которое знакомо многим любителям искусства. Данный фотограф умеет ловить моменты, запечатлевая их во всей красе.
Следующим в нашем списке идет фотограф, чьи портреты всегда полны жизни и эмоций. Его работы отличаются глубоким пониманием человека и его внутреннего мира.
Завершающим пунктом нашего обзора станет фотограф, который известен своими пейзажами. Их работы вдохновляют многих и приглашают нас в мир красоты природы.
mental health ai chatbot [url=https://mental-health21.com/]mental-health21.com[/url] .
wife whore porn dildo
Интересная статья: Марципановые пинетки своими руками: сладкий мастер-класс для начинающих
Читать полностью: Когда менять зимнюю резину: срок службы и признаки износа
ai mental health therapy [url=https://mental-health22.com/]https://mental-health22.com/[/url] .
Нужен дом? стоимость строительства дома — от проекта до отделки. Каркасные, кирпичные, брусовые, из газобетона. Гарантия качества, соблюдение сроков, индивидуальный подход.
Mental Health [url=https://mental-health23.com/]Mental Health[/url] .
Закажите уникальные изделия с индивидуальным дизайном — [url=https://pechat-na-futbolkah0.ru/]печать на футболках москва[/url] выполняется профессионально, с точной цветопередачей и гарантией стойкости изображения.
Создание дизайна на футболках позволяет подчеркнуть вашу уникальность. Технологии печати открывают широкие горизонты для дизайнеров и любителей моды.
Существует несколько популярных методов печати на футболках, каждый из которых имеет свои особенности. Например, трафаретная печать известна своей долговечностью и яркостью красок. Однако цифровая печать предоставляет больше возможностей для сложных дизайнов.
Важно помнить, что выбор ткани влияет на качество печати и долговечность изделия. Не все ткани одинаково подходят для всех технологий печати, поэтому важно подбирать материал с учетом этого.
Количество заказываемых футболок может существенно изменить ваши затраты на печать. Для небольших партий цифровая печать будет более выгодной, а для больших — трафаретная.
Weekend tweak—twitter followers buy; nice when a thread underperforms.
Friends kept asking if it’s legit to buy likes on tiktok; this exposé lays out the math.
Some sites promise big bonuses but never pay out on time. I found one of the best online casinos through Reddit and it’s been smooth and trustworthy.
Надёжный заказ авто заказать авто в россию. Машины с минимальным пробегом, отличным состоянием и по выгодной цене. Полное сопровождение: от подбора до постановки на учёт.
Полезная статья: Рецепт заливного пирога с малиной: нежная выпечка для всей семьи
Интересная новость: Яблоки запеченные с творогом в духовке: простой рецепт для всей семьи
Читать подробнее: Автоматическая коробка Aisin: стоит ли ставить на Skoda Octavia? Обзор и опыт эксплуатации
ремонт телевизоров тошиба в москве [url=https://toshiba-remont-moskva.ru/]сервисный ремонту телевизоров тошиба[/url] – профессиональный ремонт с гарантией качества.
Независимо от повода, яхта сочи аренда станет удачным решением для отдыха, фотосессии или романтического вечера на борту.
Аренда яхты — это отличный способ провести время на воде. Аренда яхт становится популярной среди туристов в теплое время года.
Получение яхты в аренду может показаться сложной задачей. Но при наличии информации, все станет намного проще.
Первым делом, вам необходимо определиться с маршрутом. Это поможет вам выбрать нужный размер и тип яхты.
Не упустите из виду условия договора аренды яхты. Знание условий аренды спасет вас от неожиданных затрат.
Если нужно заказать клининг квартиры в москве генеральную, мы подберём удобное время и выполним уборку на высоком уровне. Комфорт и чистота — наш приоритет.
Процесс генеральной уборки представляет собой важное мероприятие в бытовом обиходе. Эта процедура позволяет создавать чистоту и свежесть в жилом пространстве.
Планирование — ключ к успешной генеральной уборке. В первую очередь, нужно установить, какие зоны вы хотите убрать. Разделение на этапы поможет вам не запутаться.
Кроме того, важно подготовить необходимые средства. Чистящие средства, тряпки и пылесос — это основные вещи. Хорошая подготовка позволит сэкономить время.
После того, как все подготовлено, стоит приступать к уборке. Убирайте по одной комнате, чтобы избежать путаницы. Так будет легче увидеть результаты своих трудов.
Читать статью: Секреты пышного цветения герани: лучшие подкормки и уход
Статьи обо всем: Счастье в отношениях: как брак влияет на женское благополучие
Новое и актуальное: Секреты увлажнения кожи: натуральные средства из вашей кухни
Интересные статьи: 6 ежедневных привычек, воспитывающих счастливых и психологически устойчивых детей
купить гидромассажную ванну [url=www.hidromassazhnaya-vanna2.ru/]www.hidromassazhnaya-vanna2.ru/[/url] .
итальянская сантехника [url=www.gessi-santehnika-3.ru/]www.gessi-santehnika-3.ru/[/url] .
https://ufo.hosting/
займ взять взять онлайн займ
Читать полностью: Питание для здоровых зубов: что включить в рацион
займ онлайн бесплатно взять микрозайм
займы онлайн бесплатно микрозаймы онлайн
сантехника с доставкой [url=https://evropejskaya-santehnika.ru]https://evropejskaya-santehnika.ru[/url] .
Автомобили на заказ заказать авто из китая в россию. Работаем с крупнейшими аукционами: выбираем, проверяем, покупаем, доставляем. Машины с пробегом и без, отличное состояние, прозрачная история.
Надёжный заказ авто заказать авто в россию с аукционов: качественные автомобили, проверенные продавцы, полная сопровождение сделки. Подбор, доставка, оформление — всё под ключ. Экономия до 30% по сравнению с покупкой в РФ.
Решили заказать новый авто под ключ: подбор на аукционах, проверка, выкуп, доставка, растаможка и постановка на учёт. Честные отчёты, выгодные цены, быстрая логистика.
Хочешь авто заказать авто с аукциона? Мы поможем! Покупка на аукционе, проверка, выкуп, доставка, растаможка и ПТС — всё включено. Прямой импорт без наценок.
winline bk [url=https://www.winlayne-fribet2.ru]winline bk[/url] .
winline как получить бонус [url=https://winlayne-fribet1.ru/]https://winlayne-fribet1.ru/[/url] .
Развивайте бизнес с минимальными затратами: [url=https://lizing-auto-top77.ru/]коммерческие автомобили лизинг[/url] — это выгодный способ получить нужную технику без переплат.
Лизинг автомобилей для коммерческих нужд является выгодным решением для компаний. Лизинг дает возможность пользоваться новыми автомобилями, не тратя много средств upfront.
Поскольку лизинг обычно включает техническое обслуживание, это уменьшает финансовую нагрузку на бизнес. Это дает возможность бизнесу сосредоточиться на своих целях, а не на ремонте транспортных средств.
Клиенты также могут выбирать различные условия лизинга. Некоторые компании предлагают гибкие сроки и размеры платежей, что делает лизинг доступным для разных бизнесов.
Необходимо помнить, что лизинг транспортных средств может дать налоговые льготы. Многие предприятия могут списывать платежи по лизингу как расходы, что снижает налоговую нагрузку.
Нужна душевая кабина? интернет магазин душевых кабин: компактные и просторные модели, стеклянные и пластиковые, с глубоким поддоном и без. Установка под ключ, гарантия, помощь в подборе. Современный дизайн и доступные цены!
Поклонникам «Алых сердец», вам сюда [url=https://doramalend.online/]дорамы онлайн[/url]
888starz зеркало рабочее [url=http://888starz-casino.com.ru/]http://888starz-casino.com.ru/[/url] .
https://the.hosting/tr/help/rdp-oturumunda-masaustu-yerine-siyah-ekran
Продвижение сайта https://team-black-top.ru в ТОП Яндекса и Google. Комплексное SEO, аудит, оптимизация, контент, внешние ссылки. Рост трафика и продаж уже через 2–3 месяца.
Комедия детства один дома 1 — легендарная комедия для всей семьи. Без ограничений, в отличном качестве, на любом устройстве. Погрузитесь в атмосферу праздника вместе с Кевином!
винлайн букмекерская бонус [url=https://www.winline-fribet-za-registraciyu-2025.ru]винлайн букмекерская бонус[/url] .
Нужна душевая кабина? душевая кабина купить в минске лучшие цены, надёжные бренды, стильные решения для любой ванной. Доставка по городу, монтаж, гарантия. Каталог от эконом до премиум — найдите идеальную модель для вашего дома.
винлайн 2025 бонус за активность [url=https://www.kak-poluchit-fribet-v-winline-2025.ru]https://www.kak-poluchit-fribet-v-winline-2025.ru[/url] .
winline бонус 2025 [url=http://www.winline-fribety-2025.ru]http://www.winline-fribety-2025.ru[/url] .
как поставить бесплатную ставку на винлайн [url=www.winline-bonus-za-registraciyu-2025.ru]как поставить бесплатную ставку на винлайн[/url] .
Las [url=https://show-de-drones-0.com/]companias de espectaculos de drones[/url] combinan tecnologia de vanguardia con creatividad escenica para crear momentos que capturan la atencion desde el primer segundo.
Los shows de drones se han vuelto cada vez mas comunes en diversas celebraciones. Esos eventos con drones crean una experiencia visual impresionante que capta la atencion de grandes audiencias.
Los aparatos no tripulados permiten llevar a cabo impresionantes coreografias aereas. Esto se debe a su avanzada tecnologia y a la programacion minuciosa que los acompana.
Un aspecto clave en estos shows es la coordinacion impecable entre los diferentes drones. La combinacion de luces y movimientos crea un show impactante que maravilla a todos los asistentes.
La evolucion constante en la industria de drones augura un futuro emocionante para los espectaculos de luces y acrobacias. Proximamente, podriamos ver shows aun mas elaborados y creativos que desafian los limites de la imaginacion.
https://focusbiathlon.com/ – news about biathlon, schedule biathlon world championships and overall
winline бонус 2000 условия [url=www.besplatnyj-fribet-winline.ru/]www.besplatnyj-fribet-winline.ru/[/url] .
займы онлайн бесплатно займы
акции винлайн [url=www.winline-fribet-novym-klientam.ru]www.winline-fribet-novym-klientam.ru[/url] .
1вин [url=1win3063.ru]1вин[/url]
Архитектурное бюро официальный сайт https://arhitektura-peterburg.ru
winline bk [url=http://www.winline-fribet-kazhdyj-den.ru]winline bk[/url] .
внедрение 1с москва [url=1s-vnedrenie.ru]внедрение 1с москва[/url] .
сопровождение 1с цена [url=https://www.1s-soprovozhdenie.ru]сопровождение 1с цена[/url] .
холодильная камера для мяса купить [url=http://xn—-7sbabtdykncetibz6f4f8b.xn--p1ai/]http://xn—-7sbabtdykncetibz6f4f8b.xn--p1ai/[/url] .
внедрение erp стоимость [url=www.1s-erp-vnedrenie.ru/]внедрение erp стоимость[/url] .
аренда яхты на час [url=https://yachts-charter-dubai.com/]yachts-charter-dubai.com[/url] .
1с сопровождение цена [url=https://1s-soprovozhdenie.ru/]1с сопровождение цена[/url] .
холодильная камера цены [url=www.xn—-7sbabtdykncetibz6f4f8b.xn--p1ai/]www.xn—-7sbabtdykncetibz6f4f8b.xn--p1ai/[/url] .
камера холодильная низкотемпературная [url=http://www.xn—-7sbarc2alevbr6d.xn--p1ai]http://www.xn—-7sbarc2alevbr6d.xn--p1ai[/url] .
Решаем задачи упаковки для сложных и хрупких товаров любой конфигурации. Наш [url=https://proizvodstvo-korobok.ru/]завод картонных коробок[/url] предлагает инженерные решения.
Создание коробок играет ключевую роль в сфере упаковки. Упаковка в коробки обязательна для безопасной доставки и хранения продукции.
Коробки бывают разнообразных типов, различающихся по материалам и форм-фактору. Коробки из картона наиболее востребованы из-за своей популярности и экологичности.
Кроме того, во время производства коробок особое внимание следует уделять качеству материалов. Это обеспечит надежность упаковки и сохранность товара.
В современных условиях многие компании стремятся оптимизировать свои производственные процессы. Использование автоматизированных систем и современных технологий существенно снижает издержки.
завод картонных коробок [url=https://proizvodstvo-korobok.ru]https://proizvodstvo-korobok.ru[/url]
программа 1с цена [url=kupit-1s22.ru]программа 1с цена[/url] .
Курс по плазмолифтингу обучение prp в гинекологии в гинекологии: PRP-терапия, протоколы, показания и техника введения. Обучение для гинекологов с выдачей сертификата. Эффективный метод в эстетической и восстановительной медицине.
Курс по плазмотерапии prp терапия обучение с выдачей сертификата. Освойте PRP-методику: показания, противопоказания, протоколы, работа с оборудованием. Обучение для медработников с практикой и официальными документами.
sharp телевизор сервисный центр [url=https:/sharp-servisnyj-centr.ru/]ремонт телевизоров шарп[/url]
saif zone address spicy bite saif zone contact number
Where can I watch TV series and movies online?
Do you be informed where to wary of TV shows and films online?
Can you recommend a substantial principles to mind TV series and movies online?
[url=https://www.moviesjoy.cc/tvshows/].[/url]
прогнозы на баскетбол сегодня бесплатно [url=https://prognoz-na-segodnya-na-sport8.ru]https://prognoz-na-segodnya-na-sport8.ru[/url] .
охлаждающая камера [url=https://xn—-7sbarc2alevbr6d.xn--p1ai/]охлаждающая камера[/url] .
как приобрести программу 1с [url=http://kupit-1s21.ru]http://kupit-1s21.ru[/url] .
как приобрести программу 1с [url=https://kupit-1s22.ru]https://kupit-1s22.ru[/url] .
программа 1с цена [url=kupit-1s23.ru]программа 1с цена[/url] .
ставки на спорт прогноз [url=www.sportbets26.ru]www.sportbets26.ru[/url] .
Интересная статья: Как продлить жизнь старого автомобиля: советы и рекомендации
Читать статью: Малоподвижный образ жизни: смертельная опасность для здоровья
Интересная статья: Вишневый сок: польза для здоровья и защита от болезней
Читать в подробностях: Как повысить концентрацию и продуктивность на работе: советы психолога
Интересная новость: Как вы моетесь: неожиданные факты о характере раскроет гигиена
buy virtual number for telegram
Читать новость: Окрошка: классический рецепт на квасе и секреты приготовления
ставки на киберспорт прогнозы на сегодня [url=http://prognoz-na-segodnya-na-sport8.ru]http://prognoz-na-segodnya-na-sport8.ru[/url] .
Новое на сайте: Детские болезни: симптомы, лечение и профилактика
Launch checklist > refine bio, schedule polls, then (sparingly) buy followers on twitter before paid promos.
Новое на сайте: Яичная скорлупа: супер-удобрение для сада и комнатных растений – простой лайфхак
virtual phone number crypto
прогнозы на хоккей на сегодня от профессиональных [url=www.prognoz-na-segodnya-na-sport10.ru/]www.prognoz-na-segodnya-na-sport10.ru/[/url] .
AI platform bullbittrade.com for passive crypto trading. Robots trade 24/7, you earn. Without deep knowledge, without constant control. High speed, security and automatic strategy.
Innovative AI platform https://lumiabitai.com/ for crypto trading — passive income without stress. Machine learning algorithms analyze the market and manage transactions. Simple registration, clear interface, stable profit.
дивитися фільми як українське кіно онлайн 2025
найкращі українські фільми топ фільмів 2025 онлайн
найкращі українські фільми українські фільми онлайн HD
точный прогноз на спорт сегодня [url=https://kompyuternye-prognozy-na-futbol8.ru/]kompyuternye-prognozy-na-futbol8.ru[/url] .
стоимость аренды яхты [url=http://yachts-charter-dubai.com]http://yachts-charter-dubai.com[/url] .
прогнозы на спорт с аналитикой [url=https://prognoz-na-segodnya-na-sport10.ru/]https://prognoz-na-segodnya-na-sport10.ru/[/url] .
долгосрочная аренда яхты [url=https://yachts-charter-dubai.com/]yachts-charter-dubai.com[/url] .
прогноз на футбол с анализом [url=http://kompyuternye-prognozy-na-futbol8.ru/]http://kompyuternye-prognozy-na-futbol8.ru/[/url] .
Предлагаем [url=https://lizing-auto-top77.ru/]купить коммерческое авто в лизинг[/url] без переплат и длительного ожидания. Это решение позволит использовать транспорт в бизнесе уже сегодня.
Лизинг автомобилей для коммерческих нужд является выгодным решением для компаний. Лизинг дает возможность пользоваться новыми автомобилями, не тратя много средств upfront.
При этом, лизинг требует минимальных затрат на обслуживание. Компании могут сосредоточиться на ведении своего дела, не отвлекаясь на вопросы эксплуатации.
Клиенты также могут выбирать различные условия лизинга. Разные лизинговые компании предоставляют возможность выбора сроков договора и размеров ежемесячных взносов.
Необходимо помнить, что лизинг транспортных средств может дать налоговые льготы. Это делает лизинг еще более привлекательным для бизнеса, стремящегося минимизировать затраты.
comics 3d online comics HD online free
manga for mobile devices free colored manga site
манхва экшн лучшие манхвы
прогноз футбол на сегодня [url=http://prognozy-na-futbol-2.ru/]http://prognozy-na-futbol-2.ru/[/url] .
ремонт жк телевизоров шарп [url=https:/sharp-remont-moskva.ru/]ремонт телевизоров sharp в москве[/url]
casino giri? [url=www.candy-casino-9.com]casino giri?[/url] .
slot giri? [url=https://candy-casino-7.com]https://candy-casino-7.com[/url] .
Marca la diferencia con [url=https://show-de-drones-0.com/]la compania de espectaculos de luces con drones[/url], que transforma eventos ordinarios en recuerdos visuales extraordinarios e inolvidables.
La utilizacion de drones en espectaculos ha aumentado significativamente en la ultima decada. Estas exhibiciones ofrecen una experiencia visual unica que atrae a miles de espectadores.
Estos dispositivos voladores pueden ejecutar movimientos precisos y coordinados en el aire. Gracias a sus sofisticados sistemas de control, los drones pueden ejecutar acrobacias sorprendentes.
La sincronizacion precisa entre los aparatos voladores es uno de los rasgos mas impresionantes de estas exhibiciones. Cuando miles de drones iluminan el cielo al unisono, se crea un efecto visual que deja sin aliento.
La evolucion constante en la industria de drones augura un futuro emocionante para los espectaculos de luces y acrobacias. Proximamente, podriamos ver shows aun mas elaborados y creativos que desafian los limites de la imaginacion.
В сервисе бронирования отелей вы сможете без труда забронировать номер. Новые технологии дают возможность быстро найти и забронировать нужный отель.
[url=https://official-hotel.ru/]Забронировать отель в сервисе бронирования отелей[/url]
Выбор отеля — это важный этап подготовки к поездке. При выборе отеля следует обращать внимание на его местоположение, предлагаемые услуги и мнения клиентов.
После выбора отеля стоит внимательно ознакомиться с условиями бронирования. Не забывайте ознакомиться с условиями отмены бронирования, предоплаты и сроков проживания.
В завершение обязательно подтвердите бронь и запишите важную информацию. Тщательное внимание к каждому элементу поможет избежать неприятностей во время вашего пребывания.
casinocandy [url=http://www.candy-casino-2.com]http://www.candy-casino-2.com[/url] .
онлайн фильм 2025 аниме онлайн бесплатно
Публичная дипломатия России https://softpowercourses.ru концепции, стратегии, механизмы влияния. От культурных центров до цифровых платформ — как формируется образ страны за рубежом.
Институт государственной службы https://igs118.ru обучение для тех, кто хочет управлять, реформировать, развивать. Подготовка кадров для госуправления, муниципалитетов, законодательных и исполнительных органов.
casino giri? [url=https://candy-casino-9.com/]casino giri?[/url] .
металлические лестницы на заказ [url=www.lestnicy-na-metallokarkase-1.ru/]www.lestnicy-na-metallokarkase-1.ru/[/url] .
евросан [url=www.evropejskaya-santehnika.ru]www.evropejskaya-santehnika.ru[/url] .
Школа бизнеса EMBA https://emba-school.ru программа для руководителей и собственников. Стратегическое мышление, международные практики, управленческие навыки.
Опытный репетитор https://english-coach.ru для школьников 1–11 классов. Подтянем знания, разберёмся в трудных темах, подготовим к экзаменам. Занятия онлайн и офлайн.
Проходите аттестацию https://prom-bez-ept.ru по промышленной безопасности через ЕПТ — быстро, удобно и официально. Подготовка, регистрация, тестирование и сопровождение.
Оригинальные букеты на день рождения девушке с доставкой в Москве — это отличный способ порадовать любимую в её особенный день. Каждый цветочный букет становится настоящим произведением искусства. Наши букеты отличаются разнообразием и оригинальностью.
[url=https://bukety-na-dr.ru/]Оригинальные букеты на день рождения девушке с доставкой в Москве[/url].
Создание букета — это не только работа флориста, но и настоящая арт-терапия. Каждый цветок в букете способен отразить истинные эмоции. Подбирайте букеты, которые отражают характер вашей девушки, и мы поможем осуществить ваш выбор.
Услуга доставки цветов по Москве становится всё более популярной. Вы можете заказать доставку в любое время, и ваш сюрприз будет точно в срок. Не забывайте учитывать предпочтения вашей девушки в выборе цветов, чтобы сделать её день особенным.
Помимо традиционных цветов, можно выбрать букеты с экзотическими растениями. Необычные цветы придадут вашему подарку неповторимый шарм. Составлением букета займутся опытные флористы, чтобы ваш подарок стал лучшим.
«Дела семейные» https://academyds.ru онлайн-академия для родителей, супругов и всех, кто хочет разобраться в семейных вопросах. Психология, право, коммуникации, конфликты, воспитание — просто о важном для жизни.
Трэвел-журналистика https://presskurs.ru как превращать путешествия в публикации. Работа с редакциями, создание медийного портфолио, написание текстов, интервью, фото- и видеоматериалы.
Свежие скидки https://1001kupon.ru выгодные акции и рабочие промокоды — всё для того, чтобы тратить меньше. Экономьте на онлайн-покупках с проверенными кодами.
«Академия учителя» https://edu-academiauh.ru онлайн-портал для педагогов всех уровней. Методические разработки, сценарии уроков, цифровые ресурсы и курсы. Поддержка в обучении, аттестации и ежедневной работе в школе.
Оригинальный потолок натяжной потолок со световыми линиями со световыми линиями под заказ. Разработка дизайна, установка профиля, выбор цветовой температуры. Идеально для квартир, офисов, студий. Стильно, практично и с гарантией.
?аза? тіліндегі ?ндер Казахские хиты 2025 ж?рекке жа?ын ?уендер мен ?серлі м?тіндер. ?лтты? музыка мен ?азіргі заман?ы хиттер. Онлайн ты?дау ж?не ж?ктеу м?мкіндігі бар ы??айлы жина?.
бесплатная ставка винлайн [url=http://www.winline-fribet-novym-klientam.ru]http://www.winline-fribet-novym-klientam.ru[/url] .
купить сантехнику италия [url=https://gessi-santehnika-3.ru]https://gessi-santehnika-3.ru[/url] .
Готовый комплект Инсталляции tece с унитазом в комплекте инсталляция и унитаз — идеальное решение для современных интерьеров. Быстрый монтаж, скрытая система слива, простота в уходе и экономия места. Подходит для любого санузла.
Cost per like stayed under $0.02 when we chose to buy twitter likes cheap via Site C.
https://www.bloglovin.com/@riverafischer/findycar-goedkope-autoverhuur-wereldwijd
Простое и удобное бронирование — выберите [url=https://otdyh-dzhubga1.ru/]Джубга снять жилье[/url] заранее, чтобы ваш отпуск прошёл спокойно и без лишних забот о размещении.
Джубга считается одним из самых привлекательных курортов на Черном море. Этот курорт славится своими красивыми пляжами и мягким климатом.
В Джубге представлены разнообразные варианты размещения: от гостиниц до частного сектора. Удобные условия проживания и доступные цены делают Джубгу идеальным местом для отдыха.
Береговая линия Джубги предлагает отдыхающим прекрасные пляжи с чистым морем. Здесь можно заняться водными видами спорта или просто отдохнуть у моря с книгой.
Гастрономические удовольствия тоже составляют важную часть отдыха в Джубге. Местные рестораны славятся своим вкусным меню, включающим морепродукты и национальные блюда.
отдых в джубге [url=https://www.otdyh-dzhubga1.ru/]https://www.otdyh-dzhubga1.ru/[/url]
https://findycarpt.psee.io/7xqdeu
где находится фрибет в винлайн [url=www.winlayne-fribet.ru/]www.winlayne-fribet.ru/[/url] .
винлайн бонус за регистрацию [url=http://www.winline-fribet-kazhdyj-den.ru]http://www.winline-fribet-kazhdyj-den.ru[/url] .
купить игровой компьютер [url=https://kupit-igrovoj-kompyuter10.ru/]купить игровой компьютер[/url] .
организация онлайн трансляций москва [url=www.zakazat-onlajn-translyaciyu7.ru]www.zakazat-onlajn-translyaciyu7.ru[/url] .
игровые пк [url=https://www.kupit-igrovoj-kompyuter9.ru]игровые пк[/url] .
студия для онлайн трансляции [url=https://www.zakazat-onlajn-translyaciyu6.ru]https://www.zakazat-onlajn-translyaciyu6.ru[/url] .
стильные горшки [url=http://dizaynerskie-kashpo-sochi.ru]стильные горшки[/url] .
рулонные шторы на створку [url=https://rulonnye-shtory-s-elektroprivodom17.ru]https://rulonnye-shtory-s-elektroprivodom17.ru[/url] .
1 с бухгалтерия купить [url=https://sites.google.com/view/1s-8-buhgalteriya-bazovaya-kup/1s-8-buhgalteriya-bazovaya-kupit-kto-eshche-ne-ispolzuet-1s-v-2025-godu]1 с бухгалтерия купить[/url] .
рулонные шторы с электроприводом [url=https://rulonnye-shtory-s-elektroprivodom190.ru/]рулонные шторы с электроприводом[/url] .
рулонные шторы широкие [url=http://www.rulonnye-shtory-s-elektroprivodom17.ru]http://www.rulonnye-shtory-s-elektroprivodom17.ru[/url] .
avtozakon.online [url=www.avtozakon.online]www.avtozakon.online[/url] .
параметры трансляции [url=http://zakazat-onlajn-translyaciyu8.ru/]http://zakazat-onlajn-translyaciyu8.ru/[/url] .
Надежная защита вашего товара при транспортировке и хранении – наша специализация. [url=https://proizvodstvo-korobok.ru/]завод по производству коробок[/url] предлагает качественную упаковку любых типоразмеров под ваш продукт.
Изготовление коробок — это центральный элемент упаковочного производства. Коробки необходимы для транспортировки и хранения товаров.
Коробки бывают разнообразных типов, различающихся по материалам и форм-фактору. Самыми распространенными являются картонные коробки, которые также считаются более экологичными.
Качество материалов играет решающую роль в производстве коробок. Такой подход гарантирует устойчивость упаковки и защищенность содержимого.
Современные предприятия активно работают над улучшением своих производственных технологий. Внедрение автоматизации и инновационных технологий позволяет сократить расходы.
производитель картонных коробок москва [url=http://www.proizvodstvo-korobok.ru]http://www.proizvodstvo-korobok.ru[/url]
онлайн трансляции заказать [url=http://zakazat-onlajn-translyaciyu7.ru/]http://zakazat-onlajn-translyaciyu7.ru/[/url] .
Matthew Michael D’Agati functions as the proprietor of RW, an renewable energy Company in MA.
A couple of years of time ago, venturing into an adventurous journey, Matthew D’Agati delved into the world of solar, furthermore within a minutes commenced successfully selling significant amounts of power, mainly within the commercial industry, working with solar farm developers and local businesses in the “planning” of personal plans.
Continuous marketing just in the field, brought Matt to register a nearby start up 2 long time gone by, and in no time, he assumed the role of their Chief Strategy Officer, responsible for all functions and site building, along with being promoted social group title.
By using proper unions and shear function mentality, Matt D’Agati elevated that corporation from a marginal initially-year wages to more than a 300% build up in gross earnings by spring two. On that premise, Renewables Worldwide’s (RW), an master-held company, was shaped with the business of offering alternative fuel tips for a smarter and more environmentally friendly future.
Most really, recognizing there is a niche in the sector and an enhanced method to maintain results, RW’s is one of a handful of enterprises in the United States government to concentrate on consumer obtain, focusing in both retail and domestic solar-powered ranch off-take. Their particular image is to organize a product sales substructure on a regional, regional, countrywide level, offering a multitude of eco-friendly electrical models throughout the of Renewables Worldwide, Inc..
This passion in that the renewable sector goes on to thrill and inspire Matt in lasting his seek to work with businesses that show the the exact same of offering you alternative energy cures for a a whole lot more lasting longer term. Matthew features per in businesses from a business program at Hesser College.
[url=https://www.degreeforum.net/mybb/Thread-One-Function-of-Sustainable-Power-in-Broadening-Assortment-by-Matt-D-Agati]What does a solar broker work in Mister Whittaker framework?[/url]
[url=https://ashitamoolioli.com/4756/#comment-9154]Transitioning to Green Alternatives: Problems and Possibilities from matthew dagati[/url] 4e36bb5
Купить новогодние украшения для дома в Москве легко через интернет магазин. Такой способ оформления дома создает уникальную атмосферу праздника.
[url=https://novogodnij-dekor.ru/]Новогодние украшения для дома интернет магазин[/url]
Интернет-магазины предлагают широкий ассортимент новогодних украшений, начиная от гирлянд и заканчивая елочными игрушками. Это позволяет легко выбрать именно то, что вам нужно для вашего дома.
При покупке новогодних украшений через интернет магазин, вы также можете воспользоваться различными акциями и скидками. Так вы сможете сэкономить средства, приобретая желаемые украшения.
Удобство интернет-шопинга заключается также в возможности доставки товаров прямо к вашему дому. Вы можете заказать любимые украшения, не тратя времени на поездки по магазинам.
thmyl 1xbet akhr isdar [url=https://parimatch-apk.pro]https://parimatch-apk.pro[/url] .
I love watching the latest movies and TV shows online on MoviesJoy – it’s fast, unsolicited, and untroubled to use.
Whenever I want to moderate, I lose to MoviesJoy to runnel my favorite series and films without any hassle.
[url=https://to.moviesjoy.cc/home/]MoviesJoy[/url] is my go-to website in place of watching top-rated movies and binge-worthy shows anytime, anywhere.
[url=https://to.moviesjoy.cc/tvshows/].[/url]
data-vyhoda.online [url=www.data-vyhoda.online]www.data-vyhoda.online[/url] .
стильные вазоны [url=www.dizaynerskie-kashpo-sochi.ru]стильные вазоны[/url] .
ksusha.online [url=http://ksusha.online/]http://ksusha.online/[/url] .
У нас вы найдёте актуальные [url=https://otdyh-dzhubga1.ru/]отдых в Джубге 2025 цены[/url], которые помогут спланировать семейный отпуск без переплат. Удобное бронирование за несколько минут.
Джубга считается одним из самых привлекательных курортов на Черном море. Климат Джубги идеально подходит для пляжного отдыха и активных развлечений.
Множество отелей и пансионатов предлагают туристам различные условия для проживания. Здесь вы всегда сможете найти подходящее жилье по разумной цене.
Пляжи Джубги усыпаны мелким золотистым песком и окружены великолепной природой. Для любителей активного отдыха доступны различные водные аттракционы и экскурсии.
Кухня курорта порадует вас разнообразием блюд и свежими морепродуктами. Здесь можно попробовать блюда из свежей рыбы, а также традиционные русские и кавказские угощения.
отдых в джубге [url=http://www.otdyh-dzhubga1.ru/]http://www.otdyh-dzhubga1.ru/[/url]
lba 1xbet [url=https://parimatch-apk.pro/]https://parimatch-apk.pro/[/url] .
proedy.online [url=http://proedy.online/]http://proedy.online/[/url] .
Я малышка [url=http://imalishka.ru]http://imalishka.ru[/url] .
pelenku.ru [url=https://pelenku.ru]https://pelenku.ru[/url] .
Сайт о новорожденных детях [url=http://malishi.online]http://malishi.online[/url] .
data-vyhoda.online [url=https://data-vyhoda.online/]https://data-vyhoda.online/[/url] .
Женский журнал [url=www.ksusha.online]www.ksusha.online[/url] .
mostbet uz [url=https://mostbet4079.ru]https://mostbet4079.ru[/url]
Наша [url=https://suvenirnaya-produktsiya-spb.ru/]сувенирная продукция спб[/url] изготавливается по современным технологиям, что гарантирует долговечность и презентабельный внешний вид.
Сувенирная продукция играет важную роль в современном бизнесе. Она используется как для привлечения клиентов, так и для создания положительного имиджа.
Наиболее распространённые виды сувениров это магнитики, кружки и футболки. Каждый из этих сувениров можно адаптировать под личные предпочтения клиента, что повышает их ценность.
Приобретение сувениров нужно обдумывать, чтобы они подходили вашей целевой аудитории. Необходимо знать интересы вашей аудитории, чтобы правильно выбрать сувениры.
Рекламные стратегии, основанные на сувенирной продукции, способны увеличить продажи на несколько процентов. Сувенирная продукция, при правильном применении, может существенно увеличить лояльность клиентов.
бизнес сувениры [url=http://www.suvenirnaya-produktsiya-spb.ru/]http://www.suvenirnaya-produktsiya-spb.ru/[/url]
заказать рулонные шторы в москве [url=https://rulonnye-shtory-s-elektroprivodom11.ru/]rulonnye-shtory-s-elektroprivodom11.ru[/url] .
оригинальные цветочные горшки [url=https://dizaynerskie-kashpo-rnd.ru]оригинальные цветочные горшки[/url] .
стоимость рулонных жалюзи [url=rulonnye-elektroshtory.ru]стоимость рулонных жалюзи[/url] .
рольшторы на окна купить в москве [url=http://www.rulonnye-shtory-s-elektroprivodom11.ru]http://www.rulonnye-shtory-s-elektroprivodom11.ru[/url] .
рулонные шторы с электроприводом на окна [url=elektricheskie-rulonnye-shtory90.ru]elektricheskie-rulonnye-shtory90.ru[/url] .
Мы предлагаем клининг уборка в Москве и области, обеспечивая высокое качество, внимание к деталям и индивидуальный подход. Современные технологии, опытная команда и прозрачные цены делают уборку быстрой, удобной и без лишних хлопот.
Мы предлагаем поиск протечки в СПб и области с гарантией качества и соблюдением всех норм. Опытные мастера, современное оборудование и быстрый выезд. Честные цены, удобное время, аккуратная работа.
отзывы лечения зависимости центр лечения наркозависимых
как вывести бонусный счет с 1win [url=http://1win1161.ru]http://1win1161.ru[/url]
1win бонусы казино как использовать [url=www.1win1163.ru]www.1win1163.ru[/url]
перепланировка согласование [url=www.soglasovanie-pereplanirovki-kvartiry1.ru/]перепланировка согласование[/url] .
электропривод рулонных штор [url=zhalyuzi-s-elektroprivodom7.ru]zhalyuzi-s-elektroprivodom7.ru[/url] .
дизайнерские кашпо для цветов напольные [url=www.dizaynerskie-kashpo-nsk.ru]дизайнерские кашпо для цветов напольные[/url] .
электрокарниз купить в москве [url=www.elektrokarnizy7.ru/]www.elektrokarnizy7.ru/[/url] .
проектное бюро перепланировка квартиры [url=www.proekt-pereplanirovki-kvartiry4.ru/]www.proekt-pereplanirovki-kvartiry4.ru/[/url] .
где сделать проект перепланировки квартирым [url=https://proekt-pereplanirovki-kvartiry4.ru/]https://proekt-pereplanirovki-kvartiry4.ru/[/url] .
электрические гардины [url=https://elektrokarnizy33.ru/]elektrokarnizy33.ru[/url] .
1win app download for android [url=http://1win40011.ru/]http://1win40011.ru/[/url]
карниз с приводом для штор [url=www.elektrokarniz11.ru]www.elektrokarniz11.ru[/url] .
1win скачать на ios [url=https://www.1win40011.ru]https://www.1win40011.ru[/url]
заказ перепланировки квартиры [url=https://soglasovanie-pereplanirovki-kvartiry1.ru]https://soglasovanie-pereplanirovki-kvartiry1.ru[/url] .
электрокарнизы для штор купить [url=elektrokarnizy-dlya-shtor150.ru]elektrokarnizy-dlya-shtor150.ru[/url] .
электрокарнизы для штор купить в москве [url=https://elektrokarniz-nedorogo.ru]https://elektrokarniz-nedorogo.ru[/url] .
1вин регистрация на официальном сайте [url=http://1win1161.ru/]http://1win1161.ru/[/url]
рулонные шторы на створку [url=http://www.zhalyuzi-s-elektroprivodom7.ru]http://www.zhalyuzi-s-elektroprivodom7.ru[/url] .
joacă poker online [url=http://1win40012.ru]http://1win40012.ru[/url]
1win download ios [url=https://1win40012.ru]https://1win40012.ru[/url]
1win официальный сайт 1вин [url=www.1win1163.ru]1win официальный сайт 1вин[/url]
Сериал «Уэнсдей» https://uensdey.com мрачная и захватывающая история о дочери Гомеса и Мортиши Аддамс. Учёба в Академии Невермор, раскрытие тайн и мистика в лучших традициях Тима Бёртона. Смотреть онлайн в хорошем качестве.
Срочно нужен сантехник? https://santehnik-v-almaty.kz в Алматы? Профессиональные мастера оперативно решат любые проблемы с водопроводом, отоплением и канализацией. Доступные цены, выезд в течение часа и гарантия на все виды работ
Die Diagnose peritonealkarzinose erfordert oft eine Kombination aus operativem Eingriff und gezielter hyperthermer Chemotherapie, um Tumorherde effektiv zu entfernen und die Prognose zu verbessern.
ролет штора [url=elektricheskie-zhalyuzi.ru]elektricheskie-zhalyuzi.ru[/url] .
карнизы с электроприводом [url=https://elektrokarnizy7.ru/]elektrokarnizy7.ru[/url] .
Фильм флешка https://usb-flashki-optom-24.ru/ оптом и купить флешку в Самаре в Орле. Флешка На 8 гб цена и флешка Transcend купить в Балашихе. Колонка с флешкой оптом и блютузом купить и детская флешка купить
прокарниз [url=https://www.elektrokarnizy33.ru]https://www.elektrokarnizy33.ru[/url] .
Самая натуральная косметика http://musco.ru
Продаем оконный профиль https://okonny-profil-kupit.ru высокого качества. Большой выбор систем, подходящих для любых проектов. Консультации, доставка, гарантия.
Оконный профиль https://okonny-profil.ru купить с гарантией качества и надежности. Предлагаем разные системы и размеры, помощь в подборе и доставке. Доступные цены, акции и скидки.
рулонные шторы автоматические [url=https://www.elektricheskie-zhalyuzi.ru]https://www.elektricheskie-zhalyuzi.ru[/url] .
Use [url=https://temporary-phone-number-sms.com/]temp number[/url] to receive one-time SMS.
A temp number serves as a practical solution in many scenarios. Whether you need it for privacy concerns or online registrations, the advantages are clear.
One significant reason to use a temporary phone number is to safeguard your privacy. By employing a temp number, you can avoid unsolicited calls and messages on your real phone.
Another advantage is the ability to manage spam effectively. Registering with a personal phone number frequently results in a surge of unwanted communications.
Ultimately, utilizing a temporary number can help you maintain your privacy while enjoying online services. Consider using one the next time you need to provide a phone number online.
ремонт кофемашин на дому https://remont-kofemashin1.ru
1с бухгалтерия облако цена 1с бух облако
ремонт швейных машин на дому цена на ремонт швейных машин
автоматический карниз для штор [url=https://elektrokarnizy-dlya-shtor150.ru/]elektrokarnizy-dlya-shtor150.ru[/url] .
aviator game 1win [url=https://1win1171.ru/]aviator game 1win[/url]
1 win скачать [url=1win1166.ru]1win1166.ru[/url]
Услуга доставки тюльпанов может стать отличным подарком для любимых. Тюльпаны ассоциируются с теплом и настроением весны. Тюльпаны в качестве подарка — это всегда уместно и приятно.
Закажите [url=https://tyulpany-msk.ru/]букет из тюльпанов и радуйте своих близких свежими цветами![/url]
Существует множество видов тюльпанов с различной окраской. Каждый сорт имеет свою уникальную красоту и характер. Выбор подходящего букета для конкретного случая становится простым.
Интернет-магазины цветочной продукции предлагают доставку тюльпанов. Выбор цветов и оформление заказа через интернет могут занять всего несколько минут. Различные компании предлагают услуги по доставке тюльпанов на дом.
Доставка тюльпанов в кратчайшие сроки гарантирует радость получателю. Вы можете выбрать подходящий день и время для доставки. Не упустите шанс выбрать оригинальное оформление для своего букета.
1win мобильная версия [url=https://1win1165.ru/]https://1win1165.ru/[/url]
Купить шарики с гелием — это простое и эффектное решение для любого мероприятия. С их помощью можно легко создать праздничное настроение и атмосферу веселья.
[url=https://shariki-s-geliem.ru/]Шарики с гелием купить[/url] для вашего праздника!
Гелиевые шарики могут быть различных форм, размеров и цветов. Выбор включает как простые однотонные шарики, так и яркие с рисунками, что позволяет легко адаптировать их под ваше событие.
Купить такие шарики можно в специализированных магазинах или заказать онлайн. Заказ через интернет может быть намного удобнее и быстрее.
Не забывайте о правилах безопасности при использовании гелиевых шариков. Следите за тем, чтобы шарики не оказывались вблизи воды и всегда были под контролем.
1win промокод на деньги при пополнении [url=https://1win1169.ru]1win промокод на деньги при пополнении[/url]
1win телефон официальное приложение [url=http://1win1167.ru/]http://1win1167.ru/[/url]
1win web [url=https://www.1win40015.ru]https://www.1win40015.ru[/url]
купить стильный горшок [url=dizaynerskie-kashpo-nsk.ru]dizaynerskie-kashpo-nsk.ru[/url] .
1win ставки casino [url=https://1win40014.ru]1win ставки casino[/url]
1win телефон официальное приложение [url=https://www.1win1168.ru]https://www.1win1168.ru[/url]
слот лаки джет онлайн [url=https://www.1win1171.ru]https://www.1win1171.ru[/url]
1win букмекерская на андроид [url=www.1win1165.ru]www.1win1165.ru[/url]
1win 500% [url=https://www.1win1170.ru]https://www.1win1170.ru[/url]
как ввести промокод в 1win после регистрации [url=http://1win1166.ru]http://1win1166.ru[/url]
lucky jet регистрация [url=http://1win1167.ru]http://1win1167.ru[/url]
mobila birou chisinau [url=https://1win40015.ru/]https://1win40015.ru/[/url]
гидроизоляция цена [url=http://gidroizolyaciya-cena-2.ru]http://gidroizolyaciya-cena-2.ru[/url] .
1win зарегистрироваться [url=https://1win1169.ru/]1win зарегистрироваться[/url]
как пополнить 1win [url=https://1win1168.ru]https://1win1168.ru[/url]
Лоукост авиабилеты https://lowcost-flights.com.ua по самым выгодным ценам. Сравните предложения ведущих авиакомпаний, забронируйте онлайн и путешествуйте дешево.
Предлагаю услуги https://uslugi.yandex.ru/profile/DmitrijR-2993571 копирайтинга, SEO-оптимизации и графического дизайна. Эффективные тексты, высокая видимость в поиске и привлекательный дизайн — всё для роста вашего бизнеса.
somfy [url=https://avtomatika-somfy77.ru]somfy[/url] .
проект перепланировки в Москве [url=doskamarta.borda.ru/?1-0-0-00000089-000-0-0-1754485821]проект перепланировки в Москве [/url] .
гидроизоляция цена [url=https://gidroizolyaciya-cena-3.ru/]gidroizolyaciya-cena-3.ru[/url] .
гидроизоляция цена [url=https://www.gidroizolyaciya-cena-1.ru]https://www.gidroizolyaciya-cena-1.ru[/url] .
автоматические жалюзи с электроприводом цена [url=https://www.elektricheskie-zhalyuzi.ru]автоматические жалюзи с электроприводом цена[/url] .
гидроизоляция цена [url=www.gidroizolyaciya-cena-2.ru]www.gidroizolyaciya-cena-2.ru[/url] .
[url=https://agro-sadovod.ru/]семян семяныч официальный сайт[/url] предлагает широкий ассортимент семян и удобные условия заказа.
На сайте Семяныч размещена вся необходимая информация для клиентов. Сайт предлагает обширный ассортимент товаров и услуг, которые могут вас заинтересовать.
Также на официальном сайте Семяныч можно сделать заказ через интернет. Пользователи могут легко выбрать метод оплаты и способ доставки.
Раздел новостей на сайте всегда актуален и информативен. Здесь публикуются сведения о новых товарах и акционных предложениях.
Поддержка клиентов на сайте Семяныч работает круглосуточно. Клиенты могут получить ответы на свои вопросы и помощь в любое время.
купить аттестат об окончании 11 классов в нижнем новгороде [url=http://www.arus-diplom23.ru]купить аттестат об окончании 11 классов в нижнем новгороде[/url] .
купить диплом о высшем образовании [url=www.educ-ua5.ru/]купить диплом о высшем образовании[/url] .
аттестат 10 11 класс с реестром купить [url=http://arus-diplom24.ru]аттестат 10 11 класс с реестром купить[/url] .
АО «ГОРСВЕТ» в Чебоксарах https://gorsvet21.ru профессиональное обслуживание объектов наружного освещения. Выполняем ремонт и модернизацию светотехнического оборудования, обеспечивая комфорт и безопасность горожан.
Онлайн-сервис https://laikzaim.ru займ на карту или счет за несколько минут. Минимум документов, мгновенное одобрение, круглосуточная поддержка. Деньги в любое время суток на любые нужды.
купить диплом украины с занесением в реестр [url=www.arus-diplom34.ru/]www.arus-diplom34.ru/[/url] .
купить диплом с проводкой моих [url=http://www.arus-diplom35.ru]купить диплом с проводкой моих[/url] .
купить диплом в мурманске с занесением в реестр [url=arus-diplom35.ru]купить диплом в мурманске с занесением в реестр[/url] .
Custom Royal Portrait http://www.turnyouroyal.com an exclusive portrait from a photo in a royal style. A gift that will impress! Realistic drawing, handwork, a choice of historical costumes.
Открыть онлайн брокерский счёт – ваш первый шаг в мир инвестиций. Доступ к биржам, широкий выбор инструментов, аналитика и поддержка. Простое открытие и надёжная защита средств.
оформление перепланировки квартиры в Москве [url=http://eisberg.forum24.ru/?1-3-0-00000376-000-0-0-1754486777/]оформление перепланировки квартиры в Москве [/url] .
Букеты из тюльпанов на 8 марта — это идеальный способ выразить свои чувства и сделать этот день незабываемым. [url=https://cvety8marta.ru/]Заказать цветы к 8 марта[/url].
Тюльпановые букеты к 8 марта — это отличный способ выразить свою любовь и уважение к женщинам. Такой небольшой, но важный штрих сделает подарок еще более запоминающимся.
гидроизоляция цена [url=gidroizolyaciya-cena-3.ru]gidroizolyaciya-cena-3.ru[/url] .
bot 1win lucky jet [url=1win1174.ru]bot 1win lucky jet[/url]
ПОмощь юрист в банкротстве: юристы по банкротству юридических лиц спб
ПОмощь юрист в банкротстве: банкротство юридических лиц оказание услуг
motsbet [url=https://www.mostbet11062.ru]https://www.mostbet11062.ru[/url]
Ремонт кофемашин https://coffee-craft.kz с выездом на дом или в офис. Диагностика, замена деталей, настройка. Работаем с бытовыми и профессиональными моделями. Гарантия качества и доступные цены.
Ремонт кофемашин https://coffee-craft.kz с выездом на дом или в офис. Диагностика, замена деталей, настройка. Работаем с бытовыми и профессиональными моделями. Гарантия качества и доступные цены.
mostbet com вход [url=https://www.mostbet11061.ru]https://www.mostbet11061.ru[/url]
Круглосуточный выведение из запоев на дому — помощь на дому и в стационаре. Капельницы, очищение организма, поддержка сердца и нервной системы. Анонимно и конфиденциально.
Купить мебель стеллажи с ящиками для дома и офиса по выгодным ценам. Широкий выбор, стильный дизайн, высокое качество. Доставка и сборка по всей России. Создайте комфорт и уют с нашей мебелью.
Круглосуточный вывод из запоя с выездом на дом цена — помощь на дому и в стационаре. Капельницы, очищение организма, поддержка сердца и нервной системы. Анонимно и конфиденциально.
Купить мебель навесные шкафы для дома и офиса по выгодным ценам. Широкий выбор, стильный дизайн, высокое качество. Доставка и сборка по всей России. Создайте комфорт и уют с нашей мебелью.
сделать проект перепланировки [url=https://proekt-pereplanirovki-kvartiry5.ru/]proekt-pereplanirovki-kvartiry5.ru[/url] .
somfy [url=https://www.avtomatika-somfy77.ru]somfy[/url] .
купить аттестат за 11 класс в туле [url=www.arus-diplom24.ru/]купить аттестат за 11 класс в туле[/url] .
диплом купить реестр [url=arus-diplom34.ru]диплом купить реестр[/url] .
A friendly “ding” beats a shouted “on your left”—the rockbros bike bell is audible without being harsh, which keeps shared paths calm.
Предлагаем оконные профили https://proizvodstvo-okonnych-profiley.ru для застройщиков и подрядчиков. Высокое качество, устойчивость к климатическим нагрузкам, широкий ассортимент.
Оконные профили https://proizvodstvo-okonnych.ru для застройщиков и подрядчиков по выгодным ценам. Надёжные конструкции, современные материалы, поставка напрямую с завода.
можно ли купить диплом в реестре [url=http://www.arus-diplom34.ru]можно ли купить диплом в реестре[/url] .
Мы предлагаем документы институтов, расположенных в любом регионе Российской Федерации. Заказать диплом любого университета:
[url=http://armit.ru/social/user/42552/forum/message/2183/2185/#message2185/]купить аттестат за 11 классов дешево[/url]
Lens swaps shouldn’t require a manual; with rockbros sunglasses, they don’t. The frames flex where they should, and the lenses click in with a confident snap.
Предлагаем оконные профили https://proizvodstvo-okonnych-profiley.ru для застройщиков и подрядчиков. Высокое качество, устойчивость к климатическим нагрузкам, широкий ассортимент.
купить аттестат 11 классов за 1996 год [url=http://arus-diplom25.ru]купить аттестат 11 классов за 1996 год[/url] .
купить аттестат за 10 11 класс [url=arus-diplom22.ru]купить аттестат за 10 11 класс[/url] .
Оконные профили https://proizvodstvo-okonnych.ru для застройщиков и подрядчиков по выгодным ценам. Надёжные конструкции, современные материалы, поставка напрямую с завода.
После завершения ремонта важна [url=https://remontuborka1.ru/]клининг после ремонта спб[/url] для создания приятной и комфортной атмосферы в вашем доме.
Чистка помещений после ремонта в СПб — это важный этап, который не стоит игнорировать. Окончание ремонтных работ часто сопровождается значительным количеством грязи и остатков материалов, которые нужно убирать. Услуги профессиональной уборки сделают вашу квартиру снова уютной и чистой.
Чтобы осуществить уборку после ремонта, стоит учесть несколько факторов. Необходимо в первую очередь убрать все мусорные остатки и разобраться с отходами. Следующим этапом станет тщательная чистка всех поверхностей от пыли и загрязнений с помощью профессиональных средств.
Важно помнить, что уборка после ремонта — это не только физический труд, но и необходимость следовать определенным правилам. Если вы не хотите заниматься уборкой самостоятельно, рекомендуется обратиться к специалистам. Такой подход позволит вам сэкономить время и гарантирует высокое качество уборки.
В заключение, уборка квартир после ремонта в Санкт-Петербурге — это необходимый процесс. Игнорирование уборки может привести к неприятным последствиям для вашего жилья. Лучше всего доверить уборку после ремонта профессионалам, чтобы избежать лишних хлопот.
мостбет лицензия [url=www.mostbet11063.ru]www.mostbet11063.ru[/url]
горшок с автополивом для фиалок [url=https://www.kashpo-s-avtopolivom-kazan.ru]горшок с автополивом для фиалок[/url] .
диплом о среднем образовании купить легально [url=arus-diplom35.ru]arus-diplom35.ru[/url] .
win1 [url=http://1win1174.ru]http://1win1174.ru[/url]
помощь адвоката круглосуточно помощь адвоката
Нужны пластиковые окна: https://plastikovye-okna162.kz
Нужен вентилируемый фасад: подсистема норд фокс для вентилируемых фасадов
купить электрические рулонные шторы [url=http://elektricheskie-zhalyuzi.ru]http://elektricheskie-zhalyuzi.ru[/url] .
ремонт бойлера [url=master-remonta-boylerov.ru]master-remonta-boylerov.ru[/url]
бугуруслан купить аттестат 10 и 11 класс [url=http://www.arus-diplom21.ru]бугуруслан купить аттестат 10 и 11 класс[/url] .
mostbet сайт [url=https://mostbet11063.ru]https://mostbet11063.ru[/url]
мостбет скачать андроид [url=https://mostbet11061.ru]https://mostbet11061.ru[/url]
buy virtual number for sms verification
бк. мостбет. [url=https://mostbet11062.ru]бк. мостбет.[/url]
новости спорта [url=novosti-sporta-2.ru]novosti-sporta-2.ru[/url] .
Trust Finance https://trustf1nance.com is your path to financial freedom. Real investments, transparent conditions and stable income.
clay flowers https://www.ceramic-clay-flowers.com
Інформаційний портал https://pizzalike.com.ua про піцерії та рецепти піци в Україні й світі. Огляди закладів, адреси, меню, поради від шефів, секрети приготування та авторські рецепти. Все про піцу — від вибору інгредієнтів до пошуку найсмачнішої у вашому місті.
Trust Finance https://trustf1nance.com is your path to financial freedom. Real investments, transparent conditions and stable income.
porcelain gifts clay flowers bouquet
Інформаційний портал https://pizzalike.com.ua про піцерії та рецепти піци в Україні й світі. Огляди закладів, адреси, меню, поради від шефів, секрети приготування та авторські рецепти. Все про піцу — від вибору інгредієнтів до пошуку найсмачнішої у вашому місті.
спортивные новости [url=https://novosti-sporta-1.ru]https://novosti-sporta-1.ru[/url] .
автоматические рулонные шторы на створку [url=http://elektricheskie-zhalyuzi.ru/]http://elektricheskie-zhalyuzi.ru/[/url] .
Решили купить Honda? заказать звонок онлайн широкий ассортимент автомобилей Honda, включая новые модели, такие как Honda CR-V и Honda Pilot, а также автомобили с пробегом. Предоставляем услуги лизинга и кредитования, а также предлагает различные акции и спецпредложения для корпоративных клиентов.
Ищешь автозапчасти? оригинальные и неоригинальные автозапчасти предоставляем широкий ассортимент автозапчастей, автомобильных аксессуаров и оборудования как для владельцев легковых автомобилей, так и для корпоративных клиентов. В нашем интернет-магазине вы найдете оригинальные и неоригинальные запчасти, багажники, автосигнализации, автозвук и многое другое.
Выкуп автомобилей мощные автомобили bmw без постредников, быстро. . У нас вы можете быстро оформить заявку на кредит, продать или купить автомобиль на выгодных условиях, воспользовавшись удобным поиском по марке, модели, приводу, году выпуска и цене — независимо от того, интересует ли вас BMW, Hyundai, Toyota или другие популярные бренды.
Решили купить Honda? сервисная кампания takata широкий ассортимент автомобилей Honda, включая новые модели, такие как Honda CR-V и Honda Pilot, а также автомобили с пробегом. Предоставляем услуги лизинга и кредитования, а также предлагает различные акции и спецпредложения для корпоративных клиентов.
Ищешь автозапчасти? сервис обратной связи avto-fokus предоставляем широкий ассортимент автозапчастей, автомобильных аксессуаров и оборудования как для владельцев легковых автомобилей, так и для корпоративных клиентов. В нашем интернет-магазине вы найдете оригинальные и неоригинальные запчасти, багажники, автосигнализации, автозвук и многое другое.
привод somfy [url=www.avtomatika-somfy.ru/]www.avtomatika-somfy.ru/[/url] .
Выкуп автомобилей restyle-avto.ru/ без постредников, быстро. . У нас вы можете быстро оформить заявку на кредит, продать или купить автомобиль на выгодных условиях, воспользовавшись удобным поиском по марке, модели, приводу, году выпуска и цене — независимо от того, интересует ли вас BMW, Hyundai, Toyota или другие популярные бренды.
продвижение сайтов seo продвижение сайтов яндекс любой тематики. Поисковая оптимизация, рост органического трафика, улучшение видимости в Google и Яндекс. Работаем на результат и долгосрочный эффект.
нужен юрист: юрист по разводам Новосибирск защита интересов, составление договоров, сопровождение сделок, помощь в суде. Опыт, конфиденциальность, индивидуальный подход.
sports bet [url=https://www.sportbets32.ru]https://www.sportbets32.ru[/url] .
sport bets [url=sportbets30.ru]sportbets30.ru[/url] .
sportandbets [url=http://sportbets31.ru]http://sportbets31.ru[/url] .
free audio editor audio editing
продвижение сайтов сео яндекс любой тематики. Поисковая оптимизация, рост органического трафика, улучшение видимости в Google и Яндекс. Работаем на результат и долгосрочный эффект.
купить диплом с занесением в реестр в кемерово [url=https://arus-diplom34.ru/]https://arus-diplom34.ru/[/url] .
нужен юрист: земельный юрист Новосибирск защита интересов, составление договоров, сопровождение сделок, помощь в суде. Опыт, конфиденциальность, индивидуальный подход.
купить аттестат за 11 класс в кемерове [url=www.arus-diplom24.ru/]купить аттестат за 11 класс в кемерове[/url] .
купить аттестаты за 11 класс с отличием [url=http://www.arus-diplom24.ru]http://www.arus-diplom24.ru[/url] .
controllo volume audio dividi audio
купить аттестат за 11 класс алматы [url=https://www.arus-diplom25.ru]купить аттестат за 11 класс алматы[/url] .
Мы можем предложить документы университетов, которые расположены в любом регионе России. Заказать диплом ВУЗа:
[url=http://hitman.getbb.ru/ucp.php?mode=login&sid=b521b5aaeb527751ab3171092000bebd/]купить аттестаты за 11 класс в твери[/url]
Заказать такси https://taxi-sverdlovsk.ru онлайн быстро и удобно. Круглосуточная подача, комфортные автомобили, вежливые водители. Доступные цены, безналичная оплата, поездки по городу и за его пределы
Онлайн-заказ такси https://sverdlovsk-taxi.ru за пару кликов. Быстро, удобно, безопасно. Подача в течение 5–10 минут, разные классы авто, безналичный расчет и прозрачные тарифы.
Закажите такси https://vezem-sverdlovsk.ru круглосуточно. Быстрая подача, фиксированные цены, комфорт и безопасность в каждой поездке. Подходит для деловых, туристических и семейных поездок.
Быстрый заказ такси https://taxi-v-sverdlovske.ru онлайн и по телефону. Подача от 5 минут, комфортные автомобили, безопасные поездки. Удобная оплата и выгодные тарифы на любые направления.
купить аттестат 11 класс владивосток [url=www.arus-diplom22.ru]www.arus-diplom22.ru[/url] .
Заказать такси https://taxi-sverdlovsk.ru онлайн быстро и удобно. Круглосуточная подача, комфортные автомобили, вежливые водители. Доступные цены, безналичная оплата, поездки по городу и за его пределы
Онлайн-заказ такси https://sverdlovsk-taxi.ru за пару кликов. Быстро, удобно, безопасно. Подача в течение 5–10 минут, разные классы авто, безналичный расчет и прозрачные тарифы.
Платформа пропонує https://61000.com.ua різноманітний контент: порадник, новини, публікації на тему здоров’я, цікавих історій, місць Харкова, культурні події, архів статей та корисні матеріали для жителів міста
Закажите такси https://vezem-sverdlovsk.ru круглосуточно. Быстрая подача, фиксированные цены, комфорт и безопасность в каждой поездке. Подходит для деловых, туристических и семейных поездок.
Быстрый заказ такси https://taxi-v-sverdlovske.ru онлайн и по телефону. Подача от 5 минут, комфортные автомобили, безопасные поездки. Удобная оплата и выгодные тарифы на любые направления.
купить диплом в ровно [url=http://educ-ua4.ru/]http://educ-ua4.ru/[/url] .
диплом медсестры с занесением в реестр купить [url=https://www.arus-diplom35.ru]диплом медсестры с занесением в реестр купить[/url] .
Платформа пропонує https://61000.com.ua різноманітний контент: порадник, новини, публікації на тему здоров’я, цікавих історій, місць Харкова, культурні події, архів статей та корисні матеріали для жителів міста
купить диплом с занесением в реестр отзывы [url=http://arus-diplom32.ru/]купить диплом с занесением в реестр отзывы[/url] .
Нужен сантехник: https://santehnik-v-almaty.kz
Saznajte sve o prolom voda za bubrege – simptomi, uzroci i efikasni nacini lecenja. Procitajte savete strucnjaka i iskustva korisnika, kao i preporuke za prevenciju i brzi oporavak.
ГОРСВЕТ Чебоксары https://gorsvet21.ru эксплуатация, ремонт и установка систем уличного освещения. Качественное обслуживание, модернизация светильников и энергоэффективные решения.
Займы онлайн лайкзайм моментальное оформление, перевод на карту, прозрачные ставки. Получите нужную сумму без визита в офис и долгих проверок.
Интернет-магазин мебели https://mebelime.ru тысячи моделей для дома и офиса. Гарантия качества, быстрая доставка, акции и рассрочка. Уют в каждый дом.
спортивные новости [url=http://novosti-sporta-2.ru]http://novosti-sporta-2.ru[/url] .
Нужен сантехник: https://santehnik-v-almaty.kz
Saznajte sve o https://www.kamen-u-bubregu.com – simptomi, uzroci i efikasni nacini lecenja. Procitajte savete strucnjaka i iskustva korisnika, kao i preporuke za prevenciju i brzi oporavak.
ГОРСВЕТ Чебоксары https://gorsvet21.ru эксплуатация, ремонт и установка систем уличного освещения. Качественное обслуживание, модернизация светильников и энергоэффективные решения.
Займы онлайн лайк займ моментальное оформление, перевод на карту, прозрачные ставки. Получите нужную сумму без визита в офис и долгих проверок.
Интернет-магазин мебели https://mebelime.ru тысячи моделей для дома и офиса. Гарантия качества, быстрая доставка, акции и рассрочка. Уют в каждый дом.
Приобрести диплом о высшем образовании!
Мы изготавливаем дипломы любой профессии по выгодным ценам— [url=http://institute-diplom.ru/]institute-diplom.ru[/url]
Купить диплом под заказ в столице можно через сайт компании. [url=http://tangler.5nx.ru/posting.php?mode=post&f=3/]tangler.5nx.ru/posting.php?mode=post&f=3[/url]
форум общения знакомств как не быть обманутым при знакомствах Советы были очень дельными и существенными, помогли человеку на все 100проц, теперь он подкован, наши посетителя форума молодцы.
Zasto se javlja https://www.bol-u-bubrezima.com: od kamenaca i infekcija do prehlade. Kako prepoznati opasne simptome i brzo zapoceti lecenje. Korisne informacije.
купить аттестат об окончании 11 класса [url=www.arus-diplom21.ru/]www.arus-diplom21.ru/[/url] .
новости спорта [url=http://novosti-sporta-1.ru/]http://novosti-sporta-1.ru/[/url] .
новости спорта [url=http://novosti-sporta-2.ru/]http://novosti-sporta-2.ru/[/url] .
форум общения тренировать ягодичные мышцы способы тренировок фотоотчет, как все сделать правильно, минусы и плюсы, но тренировать нужно, здоровье дело важное.
Авто журнал https://bestauto.kyiv.ua свежие новости автопрома, тест-драйвы, обзоры новинок, советы по уходу за автомобилем и репортажи с автособытий.
Sta znaci pesak u bubrezima, koji simptomi ukazuju na problem i kako ga se resiti. Efikasni nacini lecenja i prevencije.
Популярный авто журнал https://mirauto.kyiv.ua подробные обзоры моделей, советы экспертов, новости автосалонов и автоспорта, полезные статьи для автовладельцев.
Zasto se javlja https://www.bol-u-bubrezima.com: od kamenaca i infekcija do prehlade. Kako prepoznati opasne simptome i brzo zapoceti lecenje. Korisne informacije.
Авто журнал https://bestauto.kyiv.ua свежие новости автопрома, тест-драйвы, обзоры новинок, советы по уходу за автомобилем и репортажи с автособытий.
Sta znaci pesak u bubrezima, koji simptomi ukazuju na problem i kako ga se resiti. Efikasni nacini lecenja i prevencije.
Популярный авто журнал https://mirauto.kyiv.ua подробные обзоры моделей, советы экспертов, новости автосалонов и автоспорта, полезные статьи для автовладельцев.
новости спорта [url=http://novosti-sporta-3.ru/]http://novosti-sporta-3.ru/[/url] .
лучшие прогнозы на спорт [url=https://www.prognozy-ot-professionalov.ru]лучшие прогнозы на спорт[/url] .
Флешка оптом https://usb-flashki-optom-24.ru 512 и цена флешка 16 гб в Волжском. Флешка На 4 гб купить и 32 гб флешка в Новороссийске. Игровая флешка оптом и флешка со сканером отпечатка пальца Tactum
Экономические новости https://gau.org.ua прогнозы и обзоры. Политика, бизнес, финансы, мировые рынки. Всё, что важно знать для принятия решений.
Мужской портал https://hooligans.org.ua всё, что интересно современному мужчине: стиль, спорт, здоровье, карьера, автомобили, технологии и отдых. Полезные статьи и советы каждый день.
Онлайн авто портал https://avtomobilist.kyiv.ua с обзорами новых и подержанных авто, тест-драйвами, советами по обслуживанию и новостями из мира автопрома.
Usb флешка usb-flashki-optom-24.ru/ оптом 64 гб и флешка U3 в Пскове. Мини флешка 16 гб цена и купить мини флешку в Комсомольске-на-Амуре. Флешка оптом пнг и флешки ручной работы
Экономические новости https://gau.org.ua прогнозы и обзоры. Политика, бизнес, финансы, мировые рынки. Всё, что важно знать для принятия решений.
Мужской портал https://hooligans.org.ua всё, что интересно современному мужчине: стиль, спорт, здоровье, карьера, автомобили, технологии и отдых. Полезные статьи и советы каждый день.
Онлайн авто портал https://avtomobilist.kyiv.ua с обзорами новых и подержанных авто, тест-драйвами, советами по обслуживанию и новостями из мира автопрома.
freight nyc delivery new york
прогнозы от профессионалов [url=www.prognozy-ot-professionalov1.ru/]прогнозы от профессионалов[/url] .
sportandbets [url=http://sportbets30.ru/]http://sportbets30.ru/[/url] .
Строительный портал https://dki.org.ua всё о строительстве и ремонте: технологии, оборудование, материалы, идеи для дома. Новости отрасли и экспертные рекомендации.
Портал о строительстве https://juglans.com.ua свежие новости, статьи и советы. Обзоры технологий, материалов, дизайн-идеи и практические рекомендации для профессионалов и частных застройщиков.
Онлайн строительный https://texha.com.ua портал о материалах, проектах и технологиях. Всё о ремонте, строительстве и обустройстве дома. Поддержка специалистов и вдохновение для новых идей.
Всё о стройке https://mramor.net.ua полезные статьи, советы, обзоры материалов и технологий. Ремонт, строительство домов, дизайн интерьера и современные решения для вашего проекта.
Сайт «Всё о стройке» https://sushico.com.ua подробные инструкции, советы экспертов, новости рынка. Всё о строительстве, ремонте и обустройстве жилья в одном месте.
Портал о строительстве https://juglans.com.ua свежие новости, статьи и советы. Обзоры технологий, материалов, дизайн-идеи и практические рекомендации для профессионалов и частных застройщиков.
Строительный портал https://dki.org.ua всё о строительстве и ремонте: технологии, оборудование, материалы, идеи для дома. Новости отрасли и экспертные рекомендации.
Онлайн строительный https://texha.com.ua портал о материалах, проектах и технологиях. Всё о ремонте, строительстве и обустройстве дома. Поддержка специалистов и вдохновение для новых идей.
Всё о стройке https://mramor.net.ua полезные статьи, советы, обзоры материалов и технологий. Ремонт, строительство домов, дизайн интерьера и современные решения для вашего проекта.
Сайт «Всё о стройке» https://sushico.com.ua подробные инструкции, советы экспертов, новости рынка. Всё о строительстве, ремонте и обустройстве жилья в одном месте.
прикольные цветочные горшки [url=http://dizaynerskie-kashpo-rnd.ru]http://dizaynerskie-kashpo-rnd.ru[/url] .
Стимпанк флешка usb-flashki-optom-24.ru оптом алиэкспресс и флешка 16 гб цена купить в Самаре. Флешки из металла Москва и флешка Twist 8 гб в Пензе. Оригинальные флешки оптом На 23 февраля и мини флешка
купить свидетельство о заключении брака [url=www.educ-ua4.ru/]www.educ-ua4.ru/[/url] .
прогноз на теннис на сегодня от профессионалов [url=http://www.prognozy-ot-professionalov1.ru]http://www.prognozy-ot-professionalov1.ru[/url] .
купить диплом о высшем образовании с занесением в реестр в калуге [url=https://arus-diplom34.ru/]купить диплом о высшем образовании с занесением в реестр в калуге[/url] .
купить диплом занесением реестр киев [url=https://www.pinshape.com/users/8554728-vadyymemelnvv#designs-tab-open]купить диплом занесением реестр киев[/url] .
sports bet [url=https://www.sportbets32.ru]https://www.sportbets32.ru[/url] .
sportandbets [url=https://sportbets31.ru]https://sportbets31.ru[/url] .
Приобрести диплом на заказ в столице вы сможете используя сайт компании. [url=http://windows1.listbb.ru/viewtopic.php?f=3&t=1682/]windows1.listbb.ru/viewtopic.php?f=3&t=1682[/url]
где купить диплом [url=www.educ-ua1.ru/]где купить диплом[/url] .
где можно купить аттестат за 11 [url=www.arus-diplom21.ru/]где можно купить аттестат за 11[/url] .
купить аттестат егэ 11 класс [url=https://www.arus-diplom23.ru]купить аттестат егэ 11 класс[/url] .
купить аттестат за 11 класс красноярск [url=www.arus-diplom21.ru]www.arus-diplom21.ru[/url] .
купить аттестат 11 кл в спб [url=arus-diplom22.ru]купить аттестат 11 кл в спб[/url] .
купить проведенный диплом в красноярске [url=https://arus-diplom33.ru]https://arus-diplom33.ru[/url] .
купить диплом регистрацией [url=https://arus-diplom34.ru]купить диплом регистрацией[/url] .
купить аттестат за 11 класс в школе [url=www.arus-diplom9.ru/]купить аттестат за 11 класс в школе[/url] .
диплом высшего образования с занесением в реестр купить [url=http://arus-diplom31.ru/]диплом высшего образования с занесением в реестр купить[/url] .
железобетонные прогнозы на спорт [url=www.prognozy-ot-professionalov.ru]www.prognozy-ot-professionalov.ru[/url] .
купить проведенный диплом красноярск [url=https://arus-diplom35.ru]купить проведенный диплом красноярск[/url] .
диплом с реестром купить [url=https://arus-diplom33.ru/]диплом с реестром купить[/url] .
купить аттестат за 11 класс цена [url=www.arus-diplom24.ru/]купить аттестат за 11 класс цена[/url] .
прогнозы хоккей [url=https://www.luchshie-prognozy-na-khokkej13.ru]прогнозы хоккей[/url] .
купить аттестаты за 11 класс в москве [url=https://arus-diplom25.ru]купить аттестаты за 11 класс в москве[/url] .
купить диплом в уфе с реестром [url=https://arus-diplom32.ru/]https://arus-diplom32.ru/[/url] .
инъектирование [url=https://www.remontmechty.ru/remont/inekcionnaya-gidroizolyaciya-effektivnaya-zashhita-ot-vlagi ]https://www.remontmechty.ru/remont/inekcionnaya-gidroizolyaciya-effektivnaya-zashhita-ot-vlagi [/url] .
Мы можем предложить документы университетов, расположенных на территории всей РФ. Заказать диплом любого университета:
[url=http://obrezanie05.ru/users/15/]купить аттестат 11 классов спб[/url]
мостбет войти [url=http://mostbet11069.ru]http://mostbet11069.ru[/url]
купить аттестат 11 классов в спб [url=https://www.arus-diplom22.ru]купить аттестат 11 классов в спб[/url] .
Универсальный автопортал https://road.kyiv.ua автомобили, автоновости, обзоры, ремонт, обслуживание и tuning. Полезные статьи для водителей и экспертов автоиндустрии.
Универсальный автопортал https://road.kyiv.ua автомобили, автоновости, обзоры, ремонт, обслуживание и tuning. Полезные статьи для водителей и экспертов автоиндустрии.
купить аттестат 11 классов ставрополь [url=www.arus-diplom24.ru/]купить аттестат 11 классов ставрополь[/url] .
мостбеь [url=https://www.mostbet11068.ru]https://www.mostbet11068.ru[/url]
прогноз на спорт футбол на сегодня точный [url=www.kompyuternye-prognozy-na-futbol14.ru/]www.kompyuternye-prognozy-na-futbol14.ru/[/url] .
купить диплом с проводкой моих [url=arus-diplom34.ru]купить диплом с проводкой моих[/url] .
сколько стоит купить диплом [url=https://www.educ-ua5.ru]сколько стоит купить диплом[/url] .
Женский портал https://fotky.com.ua с полезными статьями о красоте, моде, здоровье, отношениях и карьере. Советы экспертов, лайфхаки для дома, рецепты и вдохновение для каждой женщины.
Онлайн женский портал https://martime.com.ua новости, тренды моды, секреты красоты, психология отношений, карьера и семья. Полезные материалы и практические советы для женщин.
Женский портал https://fotky.com.ua с полезными статьями о красоте, моде, здоровье, отношениях и карьере. Советы экспертов, лайфхаки для дома, рецепты и вдохновение для каждой женщины.
Онлайн женский портал https://martime.com.ua новости, тренды моды, секреты красоты, психология отношений, карьера и семья. Полезные материалы и практические советы для женщин.
mostbet website [url=http://mostbet11072.ru]http://mostbet11072.ru[/url]
мостбет вход регистрация [url=http://mostbet11075.ru]http://mostbet11075.ru[/url]
прогнозы на форы в хоккее [url=luchshie-prognozy-na-khokkej13.ru]luchshie-prognozy-na-khokkej13.ru[/url] .
mostbet app login [url=www.mostbet11071.ru]www.mostbet11071.ru[/url]
мостбет кыргызстан скачать [url=https://www.mostbet11074.ru]https://www.mostbet11074.ru[/url]
Приобрести диплом о высшем образовании!
Мы изготавливаем дипломы любых профессий по приятным тарифам— [url=http://diplom4you.com/]diplom4you.com[/url]
mostbet casino скачать [url=mostbet11070.ru]mostbet11070.ru[/url]
Женский сайт https://womanclub.in.ua о красоте, моде, здоровье и стиле жизни. Полезные советы, рецепты, тренды, отношения и карьера. Всё самое интересное для женщин в одном месте.
Всё о гипертонии https://gipertoniya.net что это за болезнь, как проявляется и чем опасна. Подробные статьи о симптомах, диагностике и способах лечения высокого давления.
Туристический портал https://elnik.kiev.ua с актуальными новостями, маршрутами и путеводителями. Обзоры стран и городов, советы путешественникам, лучшие идеи для отдыха и выгодные предложения.
Женский сайт https://womanclub.in.ua о красоте, моде, здоровье и стиле жизни. Полезные советы, рецепты, тренды, отношения и карьера. Всё самое интересное для женщин в одном месте.
Онлайн женский https://ledis.top сайт о стиле, семье, моде и здоровье. Советы экспертов, обзоры новинок, рецепты и темы для вдохновения. Пространство для современных женщин.
Всё о гипертонии https://gipertoniya.net что это за болезнь, как проявляется и чем опасна. Подробные статьи о симптомах, диагностике и способах лечения высокого давления.
Туристический портал https://elnik.kiev.ua с актуальными новостями, маршрутами и путеводителями. Обзоры стран и городов, советы путешественникам, лучшие идеи для отдыха и выгодные предложения.
Онлайн женский https://ledis.top сайт о стиле, семье, моде и здоровье. Советы экспертов, обзоры новинок, рецепты и темы для вдохновения. Пространство для современных женщин.
ванна гидромассажная купить [url=http://vanna-s-gidromassazhem.ru/]http://vanna-s-gidromassazhem.ru/[/url] .
Сайт о строительстве https://stinol.com.ua практические рекомендации, проекты, обзоры инструментов и материалов. Советы экспертов, новости отрасли и новые технологии.
Строительный журнал https://mts-slil.info с актуальными новостями отрасли, обзорами материалов, инструкциями по ремонту и строительству. Полезные советы для специалистов и частных застройщиков.
Онлайн сайт https://purr.org.ua о строительстве и ремонте: полезные статьи, инструкции, обзоры технологий, дизайн-идеи и архитектурные решения для вашего дома.
Онлайн туристический https://azst.com.ua портал: всё о путешествиях, туризме и отдыхе. Маршруты, отели, лайфхаки для туристов, актуальные цены и интересные статьи о странах.
как зарегистрироваться в мостбет [url=https://mostbet11073.ru/]https://mostbet11073.ru/[/url]
Сайт о строительстве https://stinol.com.ua практические рекомендации, проекты, обзоры инструментов и материалов. Советы экспертов, новости отрасли и новые технологии.
Строительный журнал https://mts-slil.info с актуальными новостями отрасли, обзорами материалов, инструкциями по ремонту и строительству. Полезные советы для специалистов и частных застройщиков.
Онлайн сайт https://purr.org.ua о строительстве и ремонте: полезные статьи, инструкции, обзоры технологий, дизайн-идеи и архитектурные решения для вашего дома.
mostbet.kg [url=www.mostbet11069.ru]mostbet.kg[/url]
Онлайн туристический https://azst.com.ua портал: всё о путешествиях, туризме и отдыхе. Маршруты, отели, лайфхаки для туристов, актуальные цены и интересные статьи о странах.
прогнозы на исходы хоккейных матчей [url=https://luchshie-prognozy-na-khokkej13.ru]https://luchshie-prognozy-na-khokkej13.ru[/url] .
shipping services nyc trucking in nyc
Онлайн новостной https://antifa-action.org.ua портал с круглосуточным обновлением. Свежие новости, репортажи и обзоры. Важные события страны и мира, мнения экспертов и актуальная аналитика.
Новости Украины https://uamc.com.ua новости дня, аналитика, события регионов и мира. Обзоры, интервью, мнения экспертов. Быстро, достоверно и удобно для читателей.
Новостной портал https://prp.org.ua с актуальной информацией о событиях в России и мире. Политика, экономика, культура, спорт и технологии. Новости 24/7, аналитика и комментарии экспертов.
Строительный портал https://suli-company.org.ua с актуальными новостями, обзорами материалов, проектами и инструкциями. Всё о ремонте, строительстве и дизайне.
Онлайн новостной https://antifa-action.org.ua портал с круглосуточным обновлением. Свежие новости, репортажи и обзоры. Важные события страны и мира, мнения экспертов и актуальная аналитика.
Новости Украины https://uamc.com.ua новости дня, аналитика, события регионов и мира. Обзоры, интервью, мнения экспертов. Быстро, достоверно и удобно для читателей.
Новостной портал https://prp.org.ua с актуальной информацией о событиях в России и мире. Политика, экономика, культура, спорт и технологии. Новости 24/7, аналитика и комментарии экспертов.
Строительный портал https://suli-company.org.ua с актуальными новостями, обзорами материалов, проектами и инструкциями. Всё о ремонте, строительстве и дизайне.
скачать мостбет на андроид [url=http://mostbet11068.ru/]скачать мостбет на андроид[/url]
купить аттестат 11 классов 2012 [url=www.arus-diplom21.ru/]купить аттестат 11 классов 2012[/url] .
мобильное приложение регистрация вход mostbet app приложении рейтинг 4 8 [url=http://mostbet11075.ru/]http://mostbet11075.ru/[/url]
диплом колледжа купить с занесением в реестр [url=www.arus-diplom34.ru/]диплом колледжа купить с занесением в реестр[/url] .
спорт футбол прогнозы на матч [url=www.kompyuternye-prognozy-na-futbol14.ru/]www.kompyuternye-prognozy-na-futbol14.ru/[/url] .
Мы готовы предложить документы ВУЗов, расположенных на территории всей Российской Федерации. Заказать диплом о высшем образовании:
[url=http://blogger-mania.mn.co/posts/87269414/]купить аттестаты 11 класс цена[/url]
скачать официальное приложение мостбет [url=https://mostbet11067.ru]https://mostbet11067.ru[/url]
купить диплом высшего образования с занесением в реестр [url=arus-diplom35.ru]купить диплом высшего образования с занесением в реестр[/url] .
новости тенниса [url=http://novosti-sporta-11.ru]новости тенниса[/url] .
аттестат за 11 купить в нижнем новгороде [url=http://arus-diplom22.ru]аттестат за 11 купить в нижнем новгороде[/url] .
Портал про авто https://prestige-avto.com.ua обзоры новых и подержанных машин, тест-драйвы, рынок автомобилей, страхование и обслуживание.
Онлайн автомобильный https://avtonews.kyiv.ua портал: свежие автоновости, сравнительные тесты, статьи о ремонте и тюнинге. Обзоры новых и подержанных машин, цены и советы экспертов.
Современный автомобильный https://mallex.info портал: автообзоры, тесты, ремонт и обслуживание, страхование и рынок. Всё, что нужно водителям и любителям автомобилей.
Портал про авто https://prestige-avto.com.ua обзоры новых и подержанных машин, тест-драйвы, рынок автомобилей, страхование и обслуживание.
Автомобильный портал https://autonovosti.kyiv.ua новости автопрома, обзоры моделей, тест-драйвы и советы по эксплуатации. Всё для автолюбителей: от выбора авто до обслуживания и ремонта.
инъектирование [url=http://remontmechty.ru/remont/inekcionnaya-gidroizolyaciya-effektivnaya-zashhita-ot-vlagi /]http://remontmechty.ru/remont/inekcionnaya-gidroizolyaciya-effektivnaya-zashhita-ot-vlagi /[/url] .
Онлайн автомобильный https://avtonews.kyiv.ua портал: свежие автоновости, сравнительные тесты, статьи о ремонте и тюнинге. Обзоры новых и подержанных машин, цены и советы экспертов.
Современный автомобильный https://mallex.info портал: автообзоры, тесты, ремонт и обслуживание, страхование и рынок. Всё, что нужно водителям и любителям автомобилей.
Строительный сайт https://novostroi.in.ua с полезными статьями о ремонте, отделке и дизайне. Обзоры стройматериалов, проекты домов, инструкции и советы экспертов для профессионалов и новичков.
Автомобильный портал https://autonovosti.kyiv.ua новости автопрома, обзоры моделей, тест-драйвы и советы по эксплуатации. Всё для автолюбителей: от выбора авто до обслуживания и ремонта.
Строительный сайт https://novostroi.in.ua с полезными статьями о ремонте, отделке и дизайне. Обзоры стройматериалов, проекты домов, инструкции и советы экспертов для профессионалов и новичков.
как купить проведенный диплом отзывы [url=http://arus-diplom31.ru/]http://arus-diplom31.ru/[/url] .
мастбет [url=https://mostbet11071.ru]https://mostbet11071.ru[/url]
купить аттестаты за 11 в челябинске [url=https://www.arus-diplom24.ru]купить аттестаты за 11 в челябинске[/url] .
прогнозы на хоккей с высокой проходимостью [url=luchshie-prognozy-na-khokkej13.ru]luchshie-prognozy-na-khokkej13.ru[/url] .
купить диплом с занесением реестра [url=https://www.arus-diplom32.ru]купить диплом с занесением реестра[/url] .
купить диплом с записью в реестре [url=arus-diplom33.ru]купить диплом с записью в реестре[/url] .
Портал для родителей https://detiwki.com.ua и детей — всё для счастливой семьи. Воспитание, образование, здоровье, отдых и полезные материалы для мам, пап и малышей.
Сайт для женщин https://stylewoman.kyiv.ua с интересными статьями о моде, красоте, семье и здоровье. Идеи для кулинарии, путешествий и вдохновения.
Журнал садовода https://mts-agro.com.ua полезные советы по уходу за садом и огородом. Сезонные работы, выращивание овощей, фруктов и цветов, современные технологии и секреты урожая.
Универсальный сайт https://virginvirtual.net для женщин — секреты красоты, тренды моды, советы по отношениям и карьере, рецепты и стиль жизни.
Портал для родителей https://detiwki.com.ua и детей — всё для счастливой семьи. Воспитание, образование, здоровье, отдых и полезные материалы для мам, пап и малышей.
Сайт для женщин https://gratransymas.com о красоте, моде, здоровье и стиле жизни. Полезные советы, рецепты, тренды, отношения и карьера.
Универсальный сайт https://virginvirtual.net для женщин — секреты красоты, тренды моды, советы по отношениям и карьере, рецепты и стиль жизни.
Сайт для женщин https://stylewoman.kyiv.ua с интересными статьями о моде, красоте, семье и здоровье. Идеи для кулинарии, путешествий и вдохновения.
Журнал садовода https://mts-agro.com.ua полезные советы по уходу за садом и огородом. Сезонные работы, выращивание овощей, фруктов и цветов, современные технологии и секреты урожая.
умный цветочный горшок [url=www.kashpo-s-avtopolivom-kazan.ru]умный цветочный горшок[/url] .
Сайт для женщин https://gratransymas.com о красоте, моде, здоровье и стиле жизни. Полезные советы, рецепты, тренды, отношения и карьера.
Сайт обо всём https://vybir.kiev.ua энциклопедия для повседневной жизни. Красота, здоровье, дом, путешествия, карьера, семья и полезные советы для всех.
Студия дизайна https://lbook.com.ua интерьера и архитектуры. Создаём стильные проекты квартир, домов и офисов. Индивидуальный подход, современные решения и полный контроль реализации.
Портал про ремонт https://hydromech.kiev.ua свежие статьи о ремонте и отделке, дизайне интерьера и выборе материалов. Полезные советы для мастеров и тех, кто делает ремонт своими руками.
Интересный сайт https://whoiswho.com.ua обо всём: статьи, лайфхаки, обзоры и идеи на самые разные темы. Всё, что нужно для вдохновения и развития, в одном месте.
Сайт обо всём https://vybir.kiev.ua энциклопедия для повседневной жизни. Красота, здоровье, дом, путешествия, карьера, семья и полезные советы для всех.
Студия дизайна https://lbook.com.ua интерьера и архитектуры. Создаём стильные проекты квартир, домов и офисов. Индивидуальный подход, современные решения и полный контроль реализации.
Портал про ремонт https://hydromech.kiev.ua свежие статьи о ремонте и отделке, дизайне интерьера и выборе материалов. Полезные советы для мастеров и тех, кто делает ремонт своими руками.
Интересный сайт https://whoiswho.com.ua обо всём: статьи, лайфхаки, обзоры и идеи на самые разные темы. Всё, что нужно для вдохновения и развития, в одном месте.
купить диплом вуза ссср [url=http://www.educ-ua2.ru]купить диплом вуза ссср[/url] .
Онлайн портал https://esi.com.ua про ремонт: идеи для интерьера, подбор материалов, практические рекомендации и пошаговые инструкции для самостоятельных работ.
купить диплом бакалавра [url=http://educ-ua3.ru]купить диплом бакалавра[/url] .
Онлайн портал https://esi.com.ua про ремонт: идеи для интерьера, подбор материалов, практические рекомендации и пошаговые инструкции для самостоятельных работ.
Приобрести диплом на заказ в Москве возможно через сайт компании. [url=http://meetspot.com/blogs_write.php?id=/]meetspot.com/blogs_write.php?id=[/url]
Репортажи в больших https://infotolium.com фотографиях: самые обсуждаемые события, уникальные кадры и впечатляющие истории. Новости и жизнь в формате визуального рассказа.
Информационный портал https://reklama-region.com про ремонт: ремонт квартир, домов, офисов. Практические рекомендации, современные решения и обзоры стройматериалов.
Репортажи в больших https://infotolium.com фотографиях: самые обсуждаемые события, уникальные кадры и впечатляющие истории. Новости и жизнь в формате визуального рассказа.
Сайт про авто https://autoinfo.kyiv.ua свежие новости автопрома, обзоры моделей, тест-драйвы и советы по эксплуатации. Всё о машинах для водителей и автолюбителей.
Информационный портал https://reklama-region.com про ремонт: ремонт квартир, домов, офисов. Практические рекомендации, современные решения и обзоры стройматериалов.
Сайт про авто https://autoinfo.kyiv.ua свежие новости автопрома, обзоры моделей, тест-драйвы и советы по эксплуатации. Всё о машинах для водителей и автолюбителей.
последние новости спорта [url=http://novosti-sporta-12.ru/]http://novosti-sporta-12.ru/[/url] .
результаты матчей [url=www.novosti-sporta-11.ru]результаты матчей[/url] .
Сайт про автомобили https://black-star.com.ua новинки рынка, цены, тест-драйвы и обзоры. Советы экспертов по выбору и уходу за машиной, тюнинг и автоуслуги.
Онлайн-журнал https://autoiceny.com.ua для автолюбителей: автомобили, новости индустрии, тест-драйвы, тюнинг и советы по обслуживанию.
Автомобильный онлайн-журнал https://allauto.kyiv.ua свежие новости автопрома, тест-драйвы, обзоры новых моделей, советы по эксплуатации и ремонту. Всё для водителей и автолюбителей.
Сайт про автомобили https://black-star.com.ua новинки рынка, цены, тест-драйвы и обзоры. Советы экспертов по выбору и уходу за машиной, тюнинг и автоуслуги.
Автомобильный онлайн-журнал https://allauto.kyiv.ua свежие новости автопрома, тест-драйвы, обзоры новых моделей, советы по эксплуатации и ремонту. Всё для водителей и автолюбителей.
Онлайн-журнал https://autoiceny.com.ua для автолюбителей: автомобили, новости индустрии, тест-драйвы, тюнинг и советы по обслуживанию.
Royal portraits https://www.turnyouroyal.com from photos – turn yourself or your loved ones into a king, queen or aristocrat. Author’s work of artists, luxurious style and premium quality of printing.
Royal portraits http://www.turnyouroyal.com from photos – turn yourself or your loved ones into a king, queen or aristocrat. Author’s work of artists, luxurious style and premium quality of printing.
Мы предлагаем документы ВУЗов, которые находятся в любом регионе России. Купить диплом ВУЗа:
[url=http://revistaeletronica.oabrj.org.br/kupit-diplom-s-zaneseniem-v-reestr-199/]где купить аттестат за 11 класс в нижнем новгороде[/url]
как купить аттестаты за 11 класс [url=https://www.arus-diplom22.ru]как купить аттестаты за 11 класс[/url] .
купить оригинальный аттестат за 11 [url=http://arus-diplom25.ru]купить оригинальный аттестат за 11[/url] .
Авто-журнал https://bestauto.kyiv.ua источник информации для автолюбителей. Новинки рынка, сравнения моделей, советы по ремонту и уходу, интересные материалы о мире автомобилей.
Новостной портал https://gau.org.ua круглосуточные новости, комментарии экспертов, события регионов и мира. Политика, бизнес, культура и общество.
Авто-журнал https://bestauto.kyiv.ua источник информации для автолюбителей. Новинки рынка, сравнения моделей, советы по ремонту и уходу, интересные материалы о мире автомобилей.
Новостной портал https://gau.org.ua круглосуточные новости, комментарии экспертов, события регионов и мира. Политика, бизнес, культура и общество.
Онлайн авто-журнал https://mirauto.kyiv.ua с актуальными новостями, аналитикой и обзорами. Тесты автомобилей, тюнинг, технологии и советы по эксплуатации.
Авто портал https://avtomobilist.kyiv.ua всё об автомобилях: новые модели, цены, рынок подержанных авто, тюнинг и автотехнологии. Полезные материалы для автовладельцев.
Мужской портал https://hooligans.org.ua новости, лайфхаки, обзоры техники, спорт, здоровье и авто. Советы для уверенной и гармоничной жизни.
Авто портал https://avtomobilist.kyiv.ua всё об автомобилях: новые модели, цены, рынок подержанных авто, тюнинг и автотехнологии. Полезные материалы для автовладельцев.
Онлайн авто-журнал https://mirauto.kyiv.ua с актуальными новостями, аналитикой и обзорами. Тесты автомобилей, тюнинг, технологии и советы по эксплуатации.
Мужской портал https://hooligans.org.ua новости, лайфхаки, обзоры техники, спорт, здоровье и авто. Советы для уверенной и гармоничной жизни.
купить аттестаты 11 класс 2022 года [url=https://www.arus-diplom24.ru]купить аттестаты 11 класс 2022 года[/url] .
спорт сегодня [url=https://www.novosti-sporta-12.ru]спорт сегодня[/url] .
Портал о ремонте https://dki.org.ua и строительстве: от отделки квартиры до возведения загородного дома. Подробные статьи, рекомендации экспертов и идеи для обустройства жилья.
Портал о стройке https://sushico.com.ua и ремонте. Новости рынка, современные технологии, подборка идей для интерьера и экстерьера. Всё, что нужно для дома и дачи.
Онлайн сайт https://mramor.net.ua о строительстве и ремонте. Всё о возведении домов, ремонте квартир, отделке и обустройстве жилья. Обзоры материалов, советы экспертов и свежие идеи.
Портал о ремонте https://dki.org.ua и строительстве: от отделки квартиры до возведения загородного дома. Подробные статьи, рекомендации экспертов и идеи для обустройства жилья.
Портал о стройке https://sushico.com.ua и ремонте. Новости рынка, современные технологии, подборка идей для интерьера и экстерьера. Всё, что нужно для дома и дачи.
Всё о стройке https://aziatransbud.com.ua и ремонте в одном месте: дизайн, архитектура, выбор стройматериалов, инструкции по монтажу, лайфхаки и полезные рекомендации для новичков и мастеров.
Сайт о строительстве https://juglans.com.ua и ремонте — ваш помощник в выборе материалов, инструментов и технологий. Всё о ремонте квартир, строительстве домов и дизайне интерьеров.
Онлайн сайт https://mramor.net.ua о строительстве и ремонте. Всё о возведении домов, ремонте квартир, отделке и обустройстве жилья. Обзоры материалов, советы экспертов и свежие идеи.
Всё о стройке https://aziatransbud.com.ua и ремонте в одном месте: дизайн, архитектура, выбор стройматериалов, инструкции по монтажу, лайфхаки и полезные рекомендации для новичков и мастеров.
Сайт о строительстве https://juglans.com.ua и ремонте — ваш помощник в выборе материалов, инструментов и технологий. Всё о ремонте квартир, строительстве домов и дизайне интерьеров.
Онлайн журнал https://vitamax.dp.ua о строительстве: проекты домов, ремонт квартир, выбор стройматериалов, дизайн и интерьер. Советы экспертов и свежие идеи для комфортной жизни.
Портал про строительство https://texha.com.ua новости рынка, обзоры технологий, инструкции и идеи для ремонта. Материалы для застройщиков, мастеров и тех, кто делает своими руками.
футбол прогнозы [url=https://www.prognozy-na-futbol-5.ru]футбол прогнозы[/url] .
Онлайн журнал https://vitamax.dp.ua о строительстве: проекты домов, ремонт квартир, выбор стройматериалов, дизайн и интерьер. Советы экспертов и свежие идеи для комфортной жизни.
Портал про строительство https://texha.com.ua новости рынка, обзоры технологий, инструкции и идеи для ремонта. Материалы для застройщиков, мастеров и тех, кто делает своими руками.
прогноз на футбол на сегодня от профессионалов [url=https://prognozy-na-futbol-6.ru/]prognozy-na-futbol-6.ru[/url] .
Новости Украины https://gromrady.org.ua онлайн: политика, экономика, спорт, культура и события регионов. Оперативные материалы, аналитика и комментарии экспертов круглосуточно.
Новости Украины https://gromrady.org.ua онлайн: политика, экономика, спорт, культура и события регионов. Оперативные материалы, аналитика и комментарии экспертов круглосуточно.
Портал про авто https://automobile.kyiv.ua свежие новости автопрома, тест-драйвы, обзоры моделей и советы по ремонту. Всё о машинах для водителей и автолюбителей.
Авто портал https://road.kyiv.ua с актуальной информацией: новинки рынка, цены, обзоры, страхование и тюнинг. Полезные статьи и аналитика для автомобилистов.
create ringtone music editing tools
Prodaja urbanizovani placevi zabljak: stanovi, vile, zemljisne parcele. Izbor smestaja za odmor, preseljenje i investicije. Saveti strucnjaka i aktuelne ponude na trzistu.
Авто портал https://road.kyiv.ua с актуальной информацией: новинки рынка, цены, обзоры, страхование и тюнинг. Полезные статьи и аналитика для автомобилистов.
Портал про авто https://automobile.kyiv.ua свежие новости автопрома, тест-драйвы, обзоры моделей и советы по ремонту. Всё о машинах для водителей и автолюбителей.
sound editing audio online
Prodaja realitica zabljak: stanovi, vile, zemljisne parcele. Izbor smestaja za odmor, preseljenje i investicije. Saveti strucnjaka i aktuelne ponude na trzistu.
plinko slot [url=https://plinko-kz2.ru]https://plinko-kz2.ru[/url]
купить аттестат за 11 классов кемерово [url=https://www.arus-diplom21.ru]https://www.arus-diplom21.ru[/url] .
купить вкладыш аттестата 11 класс [url=www.arus-diplom22.ru]купить вкладыш аттестата 11 класс[/url] .
как вывести бонусы с 1win на карту [url=https://1win22097.ru/]https://1win22097.ru/[/url]
plinko [url=www.plinko3001.ru]plinko[/url]
спортивные прогнозы на спорт [url=http://prognozy-na-sport-8.ru/]http://prognozy-na-sport-8.ru/[/url] .
Besoin d’un bien immobilier? immobilier au Montenegro: appartements en bord de mer, maisons a la montagne, villas et appartements. Catalogue de biens, prix actuels et conseils d’experts en investissement.
ставки на футбол сегодня [url=https://prognozy-na-futbol-5.ru]https://prognozy-na-futbol-5.ru[/url] .
Besoin d’un bien immobilier? immobilier au Montenegro: appartements en bord de mer, maisons a la montagne, villas et appartements. Catalogue de biens, prix actuels et conseils d’experts en investissement.
прогноз на футбол сегодня [url=www.prognozy-na-futbol-6.ru/]прогноз на футбол сегодня[/url] .
Нужна топливная карта? топливные карты для юр лиц. Экономия до 15%, автоматическая отчётность, удобные безналичные расчёты и контроль автопарка онлайн.
Фильмы и сериалы бесплатный онлайн-кинотеатр без регистрации kinobay Онлайн-кинотеатр без регистрации и смс: тысячи фильмов и сериалов бесплатно.
plinko game online [url=www.plinko3002.ru]www.plinko3002.ru[/url]
Jak samodzielnie zdjac https://telegra.ph/Jak-samodzielnie-zdj%C4%85%C4%87-sufit-napinany-instrukcja-krok-po-kroku-bez-haka-z-wkr%C4%99tem-i-trikami-monta%C5%BCyst%C3%B3w-08-07 sufit napinany: instrukcje krok po kroku, narzedzia, porady ekspertow. Dowiedz sie, jak zdemontowac plotno bez uszkodzen i przygotowac pomieszczenie do montazu nowej okladziny.
Хотите оформить карту на топливо? https://ktz59.ru. Контроль за каждой транзакцией, отчёты для бухгалтерии, гибкие лимиты и бонусные программы.
Фильмы и сериалы Смотреть онлайн бесплатно Онлайн-кинотеатр без регистрации и смс: тысячи фильмов и сериалов бесплатно.
Jak samodzielnie zdjac https://telegra.ph/Jak-samodzielnie-zdj%C4%85%C4%87-sufit-napinany-instrukcja-krok-po-kroku-bez-haka-z-wkr%C4%99tem-i-trikami-monta%C5%BCyst%C3%B3w-08-07 sufit napinany: instrukcje krok po kroku, narzedzia, porady ekspertow. Dowiedz sie, jak zdemontowac plotno bez uszkodzen i przygotowac pomieszczenie do montazu nowej okladziny.
мелбет россия [url=https://melbet3006.com]https://melbet3006.com[/url]
салон красоты петроградская спб beauty-salon-spb.ru/
салон красоты парикмахерская https://beauty-salon-spb.ru
Нужен микрозайм? самые лучшие займы: деньги на карту без справок и поручителей. Простое оформление заявки, одобрение за минуты и мгновенное зачисление. Удобно и доступно 24/7.
Нужен микрозайм? лучшие микрозаймы онлайн: деньги на карту без справок и поручителей. Простое оформление заявки, одобрение за минуты и мгновенное зачисление. Удобно и доступно 24/7.
оценка домовладения оценочная компания
Stavki Prognozy [url=http://stavki-prognozy-two.ru]http://stavki-prognozy-two.ru[/url] .
горшок с самополивом [url=http://www.kashpo-s-avtopolivom-spb.ru]http://www.kashpo-s-avtopolivom-spb.ru[/url] .
plinko [url=https://www.plinko3002.ru]https://www.plinko3002.ru[/url]
plinko [url=https://plinko-kz2.ru]https://plinko-kz2.ru[/url]
диплом купить реестр [url=https://arus-diplom31.ru/]диплом купить реестр[/url] .
букмекерские конторы в кыргызстане [url=http://1win22097.ru]букмекерские конторы в кыргызстане[/url]
прогнозы на спорт на завтра [url=http://prognozy-na-sport-8.ru/]прогнозы на спорт на завтра[/url] .
купить диплом о высшем образовании цены украина [url=www.educ-ua4.ru/]купить диплом о высшем образовании цены украина[/url] .
Stavki Prognozy [url=stavki-prognozy-one.ru]stavki-prognozy-one.ru[/url] .
plinko kz [url=https://plinko3001.ru/]https://plinko3001.ru/[/url]
купить аттестат за 11 классов в питере [url=http://arus-diplom23.ru/]купить аттестат за 11 классов в питере[/url] .
трансформаторная подстанция ктп [url=https://www.transformatornye-podstancii-kupit2.ru]трансформаторная подстанция ктп[/url] .
аттестат об окончании 11 классов купить [url=https://www.arus-diplom22.ru]аттестат об окончании 11 классов купить[/url] .
монтаж кровли плоской крыши https://montazh-ploskoj-krovli.ru
купить диплом об окончании техникума [url=https://www.educ-ua5.ru]купить диплом об окончании техникума[/url] .
Создать документы онлайн конструктор документов word: создайте договор, заявление или акт за 5 минут. Простая форма, готовые шаблоны, юридическая точность и возможность скачать в нужном формате.
ставки прогнозы [url=https://stavki-prognozy-two.ru/]stavki-prognozy-two.ru[/url] .
купить аттестат за 11 классов в челябинской области [url=www.arus-diplom9.ru/]купить аттестат за 11 классов в челябинской области[/url] .
бесплатные высокоточные прогнозы на спорт [url=http://prognozy-na-sport-7.ru/]http://prognozy-na-sport-7.ru/[/url] .
купить аттестаты за 11 классов в новосибирске [url=www.arus-diplom23.ru]купить аттестаты за 11 классов в новосибирске[/url] .
оценка патента Москва оценочная компания
купить аттестат 11 класса 2015 года [url=http://www.arus-diplom25.ru]http://www.arus-diplom25.ru[/url] .
трансформаторные будки [url=https://www.transformatornye-podstancii-kupit.ru]https://www.transformatornye-podstancii-kupit.ru[/url] .
прогноз на хоккей на сегодня [url=www.prognozy-na-khokkej.ru/]прогноз на хоккей на сегодня[/url] .
купить диплом с проводкой моего [url=https://arus-diplom35.ru]купить диплом с проводкой моего[/url] .
купить диплом о высшем образовании с занесением в реестр отзывы [url=https://arus-diplom33.ru]купить диплом о высшем образовании с занесением в реестр отзывы[/url] .
аттестат за 11 класс купить в чите [url=https://arus-diplom24.ru/]аттестат за 11 класс купить в чите[/url] .
Авто помощь 24/7 служба помощи на дорогах: устранение поломок, подвоз топлива, прикуривание аккумулятора, замена колеса и эвакуация автомобиля.
Авто помощь 24/7 выездная техпомощь на дороге: устранение поломок, подвоз топлива, прикуривание аккумулятора, замена колеса и эвакуация автомобиля.
трансформаторная подстанция купить [url=www.transformatornye-podstancii-kupit2.ru/]трансформаторная подстанция купить[/url] .
купить аттестат за 11 класс в череповце [url=http://arus-diplom24.ru]купить аттестат за 11 класс в череповце[/url] .
блочная комплектная трансформаторная подстанция [url=http://www.transformatornye-podstancii-kupit1.ru]блочная комплектная трансформаторная подстанция[/url] .
stavkiprognozy [url=www.stavki-prognozy-one.ru]www.stavki-prognozy-one.ru[/url] .
диплом настоящий купить с занесением в реестр [url=www.arus-diplom31.ru]www.arus-diplom31.ru[/url] .
ставки прогнозы [url=https://www.stavki-prognozy-2.ru]https://www.stavki-prognozy-2.ru[/url] .
Срочно нужны купить цветы Минск Свежие букеты, праздничные композиции и эксклюзивные флористические решения. Онлайн-заказ и быстрая доставка по городу.
Профессиональные детейлинг 812detailing: полировка кузова, химчистка салона, восстановление пластика и защита керамикой. Вернём автомобилю блеск и надёжную защиту.
Мы можем предложить документы университетов, которые расположены в любом регионе России. Купить диплом о высшем образовании:
[url=http://xtrainkom.com/employer/all-diplomy/]где можно купить аттестаты 11 класс[/url]
Срочно нужны доставка цветов Свежие букеты, праздничные композиции и эксклюзивные флористические решения. Онлайн-заказ и быстрая доставка по городу.
Профессиональные детейлинг спб цена: полировка кузова, химчистка салона, восстановление пластика и защита керамикой. Вернём автомобилю блеск и надёжную защиту.
Нужен массаж? https://doctu.ru – профессиональные мастера, широкий выбор техник: классический, оздоровительный, лимфодренажный, детский. Доступные цены и уютная атмосфера.
силовые трансформаторные подстанции [url=https://transformatornye-podstancii-kupit.ru/]transformatornye-podstancii-kupit.ru[/url] .
Нужен массаж? Массаж Ивантеевка – профессиональные мастера, широкий выбор техник: классический, оздоровительный, лимфодренажный, детский. Доступные цены и уютная атмосфера.
Обучающие курсы онлайн курсы по нейросетям новые навыки для работы и жизни. IT, дизайн, менеджмент, языки, маркетинг. Гибкий график, практика и сертификаты по итогам.
купить диплом в одессе цены [url=http://educ-ua4.ru]купить диплом в одессе цены[/url] .
cheap vps hosting https://vpsserverhosting1.com
комплектные трансформаторные подстанции ктп купить [url=transformatornye-podstancii-kupit1.ru]transformatornye-podstancii-kupit1.ru[/url] .
стул для мастера педикюра лампа лупа для косметолога купить
купить аттестат за 11 класс в казани [url=http://www.arus-diplom22.ru]купить аттестат за 11 класс в казани[/url] .
мостбет лайв ставки [url=https://www.mostbet4104.ru]https://www.mostbet4104.ru[/url]
узи аппараты среднего класса [url=kupit-uzi-apparat27.ru]узи аппараты среднего класса[/url] .
узи сканер купить цена [url=https://kupit-uzi-apparat25.ru]https://kupit-uzi-apparat25.ru[/url] .
медицинское оборудование узи [url=http://kupit-uzi-apparat26.ru/]медицинское оборудование узи[/url] .
https://jsfiddle.net/findycartr/6vpjbcyL/
mostbet uz sport tikish [url=https://www.mostbet4103.ru]https://www.mostbet4103.ru[/url]
мостбет ставки на исход [url=https://www.mostbet4148.ru]https://www.mostbet4148.ru[/url]
мостбет казино [url=www.mostbet4146.ru]мостбет казино[/url]
mostbet kz скачать [url=http://mostbet4149.ru/]http://mostbet4149.ru/[/url]
бк мостбет [url=http://mostbet4150.ru/]http://mostbet4150.ru/[/url]
https://www.tapatalk.com/groups/renotalkfr/viewtopic.php?f=72&t=251986&from_new_topic=1
мостбет уз скачать [url=www.mostbet4105.ru]мостбет уз скачать[/url]
vps hosting in europe vps hosting
Мы предлагаем документы университетов, расположенных на территории всей Российской Федерации. Приобрести диплом о высшем образовании:
[url=http://vidagrafia.com/read-blog/187567/]где можно купить аттестат 11 классов в екатеринбурге[/url]
mostbet.com [url=https://mostbet4104.ru]mostbet.com[/url]
кашпо с автополивом для комнатных растений [url=https://kashpo-s-avtopolivom-spb.ru/]кашпо с автополивом для комнатных растений[/url] .
мостбет оператор [url=www.mostbet4147.ru]мостбет оператор[/url]
букмекерская контора мостбет [url=http://mostbet4148.ru]букмекерская контора мостбет[/url]
косметологический столик косметологическое кресло
https://share.evernote.com/note/5c6d19d3-b541-b197-01bc-55bad748b5a9
мед аппарат узи [url=http://www.kupit-uzi-apparat25.ru]http://www.kupit-uzi-apparat25.ru[/url] .
mostbet vxod [url=www.mostbet4103.ru]www.mostbet4103.ru[/url]
мостбет сом [url=https://www.mostbet4149.ru]https://www.mostbet4149.ru[/url]
mostbet.com rasmiy sayt [url=http://mostbet4102.ru/]http://mostbet4102.ru/[/url]
https://www.flickr.com/people/203276904@N05/
куб бетона саратов саратов купить бетон цена
Хотите заказать интро для диджея? Индивидуальная разработка музыкальных заставок для рекламы, подкастов и презентаций. Качественный звук и креатив для запоминающегося бренда.
как купить легально диплом о высшем образовании [url=https://arus-diplom31.ru/]как купить легально диплом о высшем образовании[/url] .
Наркологические услуги: капельница на дом наркологическая, кодирование, детоксикация, снятие ломки, помощь при алкоголизме и наркомании. Круглосуточная поддержка и анонимность.
mostbet texnik yordam [url=https://mostbet4105.ru/]mostbet texnik yordam[/url]
mostbet скачать на телефон [url=http://mostbet4147.ru/]http://mostbet4147.ru/[/url]
mostbet [url=https://www.mostbet4150.ru]https://www.mostbet4150.ru[/url]
Наркологические услуги: наркологическая клиника алкоголь нижний новгород, кодирование, детоксикация, снятие ломки, помощь при алкоголизме и наркомании. Круглосуточная поддержка и анонимность.
скачать мостбет казино на андроид [url=https://mostbet4146.ru/]https://mostbet4146.ru/[/url]
купить диплом о высшем образовании в запорожье [url=https://www.educ-ua1.ru]купить диплом о высшем образовании в запорожье[/url] .
Puzzle Man Pro https://apps.apple.com/ro/app/puzzle-man-pro/id455696756 exciting puzzles for iOS. Collect classic pictures or create puzzles from your own photos. Different difficulty levels, user-friendly interface and saving progress.
Свежее и интересное: https://www.sibledy.ru/thread-333786-1-1.html
как зайти на сайт melbet [url=https://www.melbetofficialsite.ru]как зайти на сайт melbet[/url] .
самые точные прогнозы на нхл [url=http://luchshie-prognozy-na-khokkej14.ru/]http://luchshie-prognozy-na-khokkej14.ru/[/url] .
гидроизоляция цена [url=https://gidroizolyaciya-cena-1.ru/]gidroizolyaciya-cena-1.ru[/url] .
Стройкаталог https://stroycata1og.ru проекты коттеджей, дома любой площади, каталог стройматериалов. Комплексные услуги от проектирования до сдачи объекта с гарантией качества.
узи аппарат цена новый [url=http://kupit-uzi-apparat28.ru]узи аппарат цена новый[/url] .
доставка бетона саратов куб бетона саратов
Block Puzzle Wood Classic https://apps.apple.com/vi/app/block-puzzle-wood-classic/id1615792350 is a puzzle game where you need to correctly place wooden blocks. Simple controls, beautiful visuals and addictive gameplay for all ages.
мелбет казино играть на деньги [url=http://melbetofficialsite.ru/]http://melbetofficialsite.ru/[/url] .
гидроизоляция цена [url=http://www.gidroizolyaciya-cena-1.ru]http://www.gidroizolyaciya-cena-1.ru[/url] .
прогнозы на периоды в хоккее [url=http://luchshie-prognozy-na-khokkej14.ru/]http://luchshie-prognozy-na-khokkej14.ru/[/url] .
мостбет бонус за регистрацию уз [url=www.mostbet4102.ru]www.mostbet4102.ru[/url]
mostbet mobile uz registratsiya [url=mostbet4111.ru]mostbet4111.ru[/url]
mostbet app ios [url=mostbet4106.ru]mostbet4106.ru[/url]
уличные горшки для цветов [url=http://www.ulichnye-kashpo-kazan.ru]уличные горшки для цветов[/url] .
mosbet [url=mostbet4109.ru]mostbet4109.ru[/url]
мостбе [url=www.mostbet4118.ru]мостбе[/url]
mostbet com android [url=https://mostbet4117.ru]mostbet com android[/url]
mostbet link [url=www.mostbet4111.ru]www.mostbet4111.ru[/url]
сантехника москва купить [url=www.gessi-santehnika-5.ru]www.gessi-santehnika-5.ru[/url] .
Handmade flower artists Ideal for home, office decor or original gift. Natural beauty and durability.
Handmade ceramics flowers Ideal for home, office decor or original gift. Natural beauty and durability.
ванная с джакузи [url=http://www.vanna-s-gidromassazhem.ru]ванная с джакузи[/url] .
mostbet uz jonli tikish [url=https://mostbet4107.ru]mostbet uz jonli tikish[/url]
Бетон в Воронеже https://stk-vrn.ru продажа и доставка. Все марки для фундаментов, дорожных работ и строительства под ключ. Надёжный производитель и лучшие цены.
мостбе [url=https://www.mostbet4147.ru]https://www.mostbet4147.ru[/url]
Бетон в Воронеже https://stk-vrn.ru продажа и доставка. Все марки для фундаментов, дорожных работ и строительства под ключ. Надёжный производитель и лучшие цены.
mostbet uz skachat kompyuter [url=http://mostbet4106.ru/]http://mostbet4106.ru/[/url]
мостбеь [url=mostbet4117.ru]mostbet4117.ru[/url]
рекламное агентство seo [url=http://rosy-rabbit-qsgmm1.mystrikingly.com/]http://rosy-rabbit-qsgmm1.mystrikingly.com/[/url] .
купить аттестат за 11 класс с занесением в реестр москва [url=https://www.arus-diplom21.ru]купить аттестат за 11 класс с занесением в реестр москва[/url] .
хочу купить аттестат 11 классов [url=http://arus-diplom22.ru]http://arus-diplom22.ru[/url] .
gessi продукция [url=https://gessi-santehnika-5.ru/]https://gessi-santehnika-5.ru/[/url] .
бк мост бет [url=http://mostbet4118.ru/]бк мост бет[/url]
mostbet.com что это [url=www.mostbet4147.ru]mostbet.com что это[/url]
недорогие гидромассажные ванны [url=https://vanna-s-gidromassazhem.ru]недорогие гидромассажные ванны[/url] .
mostbet aviator hack uz [url=https://mostbet4109.ru/]mostbet aviator hack uz[/url]
диплом о высшем образовании с занесением в реестр купить [url=http://arus-diplom31.ru]диплом о высшем образовании с занесением в реестр купить[/url] .
евросан [url=http://evropejskaya-santehnika2.ru/]http://evropejskaya-santehnika2.ru/[/url] .
нтернет-магазин сантехники https://vodomirural.ru ванны, смесители, унитазы, раковины и душевые кабины. Большой выбор, доступные цены, доставка и гарантия качества от производителей.
аттестат за 11 класс купить в новосибирске [url=http://www.arus-diplom23.ru]аттестат за 11 класс купить в новосибирске[/url] .
онлайн деньги взять деньги онлайн
купить аттестат 11 класс 2016 год [url=http://arus-diplom24.ru]купить аттестат 11 класс 2016 год[/url] .
взять займ онлайн займ онлайн бесплатно
mostbet aviator az [url=https://www.mostbet4134.ru]https://www.mostbet4134.ru[/url]
купить диплом занесением в реестр [url=https://arus-diplom31.ru]купить диплом занесением в реестр[/url] .
mostbet qanday pul yechiladi [url=mostbet4113.ru]mostbet qanday pul yechiladi[/url]
займ онлайн бесплатно займ онлайн
займ онлайн займы деньги
микрозаймы онлайн получить займ онлайн
микрозаймы онлайн деньги
мостбет приложение ios [url=mostbet4116.ru]mostbet4116.ru[/url]
mostbet aviator oyunu [url=https://mostbet4135.ru/]mostbet aviator oyunu[/url]
купить аттестат 11 классов цена [url=http://arus-diplom25.ru]купить аттестат 11 классов цена[/url] .
агентства по продвижению сайтов [url=http://www.telegra.ph/Agentstvo-po-prodvizheniyu-sajtov-chto-vazhno-znat-pered-vyborom-08-15]http://www.telegra.ph/Agentstvo-po-prodvizheniyu-sajtov-chto-vazhno-znat-pered-vyborom-08-15[/url] .
купить гидромассажную ванну [url=http://vanna-s-gidromassazhem.ru/]http://vanna-s-gidromassazhem.ru/[/url] .
mostbet tennis mərcləri [url=https://mostbet4134.ru/]mostbet tennis mərcləri[/url]
Мы можем предложить дипломы любой профессии по приятным ценам. Заказ документа, который подтверждает окончание ВУЗа, – это разумное решение. Заказать диплом университета: [url=http://neoncity.gtaserv.ru/posting.php?mode=post&f=38&sid=417cbca8685e4bea5285c5415191348c/]neoncity.gtaserv.ru/posting.php?mode=post&f=38&sid=417cbca8685e4bea5285c5415191348c[/url]
строительство домов иркутская область [url=https://stroitelstvo-domov-irkutsk-6.ru/]https://stroitelstvo-domov-irkutsk-6.ru/[/url] .
мостбет на футбол ставки [url=http://mostbet4113.ru]http://mostbet4113.ru[/url]
проекты домов под ключ [url=www.stroitelstvo-domov-irkutsk-4.ru]проекты домов под ключ[/url] .
застройщики частных домов иркутск [url=www.stroitelstvo-domov-irkutsk-2.ru/]www.stroitelstvo-domov-irkutsk-2.ru/[/url] .
mostbet akkaunt yaratish [url=http://mostbet4112.ru]http://mostbet4112.ru[/url]
Tickets for Music Festivals https://rock-concert-tickets.ru
mostbet uz ro‘yxatdan qanday o‘tish [url=www.mostbet4115.ru]mostbet uz ro‘yxatdan qanday o‘tish[/url]
Рейтинг хостингов топ хостингов в россии подбор сервисов для сайтов и интернет-магазинов. Сравнение тарифов, гарантия стабильности и рекомендации по выбору.
Buying Tickets for Concerts https://rock-concert-tickets.ru
ванна с гидромассажем [url=https://vanna-s-gidromassazhem.ru/]ванна с гидромассажем[/url] .
Рестораны Хамовников https://restoran-khamovniki.ru топ заведений для встреч, романтических ужинов и семейных обедов. Авторская кухня, стильный интерьер, удобное расположение и достойный сервис.
Лучшие рестораны https://hamovniki-restoran.ru Хамовников для ценителей гастрономии. Подборка заведений с изысканной кухней, качественным сервисом и атмосферой для отдыха и деловых встреч.
Рестораны Хамовников https://restoran-khamovniki.ru топ заведений для встреч, романтических ужинов и семейных обедов. Авторская кухня, стильный интерьер, удобное расположение и достойный сервис.
Лучшие рестораны https://hamovniki-restoran.ru Хамовников для ценителей гастрономии. Подборка заведений с изысканной кухней, качественным сервисом и атмосферой для отдыха и деловых встреч.
mostbet uz ga kirish [url=https://www.mostbet4116.ru]https://www.mostbet4116.ru[/url]
Курсы по плазмотерапии плазмолифтинг обучение в москве освоение методик, современные протоколы, практическая отработка. Обучение для специалистов с выдачей сертификата и повышением квалификации.
mostbet promo qeydiyyat [url=http://mostbet4135.ru/]http://mostbet4135.ru/[/url]
Профессиональное обучение плазмотерапия в косметологии обучение: подробная программа, практические навыки, сертификация. Освойте эффективные методики для применения в медицине и косметологии.
Курсы по плазмотерапии плазмотерапия обучение в москве освоение методик, современные протоколы, практическая отработка. Обучение для специалистов с выдачей сертификата и повышением квалификации.
Профессиональное обучение плазмолифтинг для лица обучение: подробная программа, практические навыки, сертификация. Освойте эффективные методики для применения в медицине и косметологии.
уличные кашпо для цветов купить [url=www.ulichnye-kashpo-kazan.ru/]уличные кашпо для цветов купить[/url] .
готовые дома иркутск [url=https://stroitelstvo-domov-irkutsk-6.ru]готовые дома иркутск[/url] .
мостьет [url=https://mostbet4112.ru]https://mostbet4112.ru[/url]
Заказать диплом ВУЗа можем помочь. Купить аттестат в Туле – [url=http://diplomybox.com/kupit-attestat-v-tule/]diplomybox.com/kupit-attestat-v-tule[/url]
строительство дома под ключ иркутск [url=stroitelstvo-domov-irkutsk-4.ru]stroitelstvo-domov-irkutsk-4.ru[/url] .
проекты домов под ключ [url=https://stroitelstvo-domov-irkutsk-2.ru/]проекты домов под ключ[/url] .
Мы можем предложить дипломы любой профессии по невысоким ценам. Дипломы по профессии — [url=http://kyc-diplom.com/diplomy-po-professii.html/]kyc-diplom.com/diplomy-po-professii.html[/url]
Детская школа искусств https://elegy-school.ru обучение музыке, танцам, изобразительному и театральному искусству. Творческие программы для детей, концерты, конкурсы и развитие талантов.
Авторские курсы по REVIT https://dashclass.ru обучение созданию интерьеров и архитектурных проектов. Практика, реальные кейсы, индивидуальный подход и профессиональные навыки для работы в проектировании.
Детская школа искусств https://elegy-school.ru обучение музыке, танцам, изобразительному и театральному искусству. Творческие программы для детей, концерты, конкурсы и развитие талантов.
Авторские курсы по REVIT https://dashclass.ru обучение созданию интерьеров и архитектурных проектов. Практика, реальные кейсы, индивидуальный подход и профессиональные навыки для работы в проектировании.
mostbet uz ro‘yxatdan o‘tish bonusi [url=https://mostbet4115.ru/]mostbet uz ro‘yxatdan o‘tish bonusi[/url]
pin up xavfsizmi [url=http://pinup5003.ru]http://pinup5003.ru[/url]
pin-up [url=https://pinup5002.ru/]pin-up[/url]
Первая помощь детям https://firstaidkids.ru правила оказания при травмах, ожогах, удушье и других ситуациях. Пошаговые инструкции, советы врачей и полезная информация для родителей.
Студия иностранных языков https://whats-up-studiya-inostrannyh-yazykov.ru обучение английскому, немецкому, французскому и другим языкам. Индивидуальные и групповые занятия, современные методики и опытные преподаватели.
Первая помощь детям https://firstaidkids.ru правила оказания при травмах, ожогах, удушье и других ситуациях. Пошаговые инструкции, советы врачей и полезная информация для родителей.
Студия иностранных языков https://whats-up-studiya-inostrannyh-yazykov.ru обучение английскому, немецкому, французскому и другим языкам. Индивидуальные и групповые занятия, современные методики и опытные преподаватели.
pin up promo kod 2025 uz [url=pinup5005.ru]pin up promo kod 2025 uz[/url]
mostbet-uz [url=https://www.mostbet4163.ru]mostbet-uz[/url]
купить проведенный диплом вуза [url=https://arus-diplom31.ru/]https://arus-diplom31.ru/[/url] .
Заказать диплом об образовании!
Мы изготавливаем дипломы психологов, юристов, экономистов и любых других профессий по выгодным ценам— [url=http://obrazovaie-rf.ru/]obrazovaie-rf.ru[/url]
mostbet скачать на айфон [url=mostbet4164.ru]mostbet скачать на айфон[/url]
pin up ilova orqali tikish [url=http://pinup5003.ru]http://pinup5003.ru[/url]
mostbet rasmiy sayti [url=www.mostbet4161.ru]mostbet rasmiy sayti[/url]
Срочный вызов сантехника https://master-expert.com в Москве на дом. Услуги сантехника: прочистка засоров, ремонт смесителей, установка приборов учета. Работаем 24/7. Недорого и с гарантией. Подробнее на сайте
Детский сад № 55 https://detsadik55.ru забота, развитие и обучение детей. Современные программы, квалифицированные воспитатели, уютные группы, безопасная среда и внимание к каждому ребёнку.
Срочный вызов сантехника https://master-expert.com в Москве на дом. Услуги сантехника: прочистка засоров, ремонт смесителей, установка приборов учета. Работаем 24/7. Недорого и с гарантией. Подробнее на сайте
пин ап центр помощи [url=www.pinup5002.ru]www.pinup5002.ru[/url]
Детский сад № 55 https://detsadik55.ru забота, развитие и обучение детей. Современные программы, квалифицированные воспитатели, уютные группы, безопасная среда и внимание к каждому ребёнку.
мостбет обман или нет [url=http://mostbet4163.ru/]мостбет обман или нет[/url]
Промышленная безопасность https://аттестация-промбезопасность.рф курсы и обучение под ключ. Подготовка к проверке Ростехнадзора, повышение квалификации и сертификация специалистов предприятий.
Автомобили на заказ https://avto-iz-kitaya1.ru поиск, проверка, покупка и доставка. Китай и Корея. Индивидуальный подбор под бюджет и пожелания клиента, полное сопровождение сделки.
Промышленная безопасность https://аттестация-промбезопасность.рф курсы и обучение под ключ. Подготовка к проверке Ростехнадзора, повышение квалификации и сертификация специалистов предприятий.
Автомобили на заказ https://avto-iz-kitaya1.ru поиск, проверка, покупка и доставка. Китай и Корея. Индивидуальный подбор под бюджет и пожелания клиента, полное сопровождение сделки.
pin up savollar va javoblar [url=http://pinup5001.ru/]http://pinup5001.ru/[/url]
мостбет узкард вывод [url=http://mostbet4161.ru]http://mostbet4161.ru[/url]
вывод из запоя клиника москва [url=http://www.narkologicheskaya-klinika-11.ru]http://www.narkologicheskaya-klinika-11.ru[/url] .
купить гашиш недорого где можно купить гашиш
шишки бошки меф купить метадон героин купить закладку
шишки бошки меф купить купить героин спб
купить героин амфетамин купить мефедрон гашиш
пин ап получить бонус через промо [url=http://pinup5005.ru/]http://pinup5005.ru/[/url]
Авто из Китая https://avto-iz-kitaya2.ru на заказ под ключ: подбор, проверка, доставка и растаможка. Новые и подержанные автомобили, выгодные цены и полное сопровождение сделки.
Авто из Китая https://avto-iz-kitaya2.ru на заказ под ключ: подбор, проверка, доставка и растаможка. Новые и подержанные автомобили, выгодные цены и полное сопровождение сделки.
pin up bonus olish [url=https://pinup5001.ru]https://pinup5001.ru[/url]
мостбет бонус за регистрацию уз [url=www.mostbet4164.ru]мостбет бонус за регистрацию уз[/url]
перевод договора с латышского на русский [url=www.onlineperevodchik.ru]www.onlineperevodchik.ru[/url] .
Авто из Китая под заказ https://dostavka-avto-china.ru кроссоверы, седаны, электромобили и премиальные модели. Индивидуальный подбор, проверка, сопровождение сделки и доставка в ваш город.
Автомобили из Китая на заказ https://avto-iz-kitaya2.ru подбор, покупка и доставка. Полный цикл услуг: диагностика, растаможка, постановка на учёт и гарантия качества.
Авто из Китая под заказ https://dostavka-avto-china.ru кроссоверы, седаны, электромобили и премиальные модели. Индивидуальный подбор, проверка, сопровождение сделки и доставка в ваш город.
Автомобили из Китая на заказ https://avto-iz-kitaya2.ru подбор, покупка и доставка. Полный цикл услуг: диагностика, растаможка, постановка на учёт и гарантия качества.
купить диплом проведенный [url=www.arus-diplom32.ru]купить диплом проведенный[/url] .
наркологические клиники москвы [url=www.narkologicheskaya-klinika-11.ru]www.narkologicheskaya-klinika-11.ru[/url] .
PuzzleFree online puzzles https://www.hitechwork.com/best-5-free-online-jigsaw-puzzles-for-everyone/ hundreds of pictures to assemble, different difficulty levels and user-friendly interface. Enjoy the process, train your memory and attention for free.
Заказать авто из Китая https://dostavka-avto-china2.ru новые автомобили с гарантией, выгодные цены и проверенные поставщики. Доставка, таможня и оформление всех документов под ключ.
Заказать авто из Китая https://dostavka-avto-china2.ru новые автомобили с гарантией, выгодные цены и проверенные поставщики. Доставка, таможня и оформление всех документов под ключ.
mostbet canlı yayım [url=www.mostbet4137.ru]mostbet canlı yayım[/url]
кашпо для комнатных растений напольные [url=http://www.kashpo-napolnoe-moskva.ru]http://www.kashpo-napolnoe-moskva.ru[/url] .
построить дом иркутск [url=https://www.stroitelstvo-domov-irkutsk-6.ru]построить дом иркутск[/url] .
построить дом под ключ [url=stroitelstvo-domov-irkutsk-1.ru]stroitelstvo-domov-irkutsk-1.ru[/url] .
мостбет вход через соцсети [url=https://mostbet4152.ru]https://mostbet4152.ru[/url]
перевод договора с киргизского на русский [url=http://www.onlineperevodchik.ru]http://www.onlineperevodchik.ru[/url] .
mostbet az casino [url=mostbet4140.ru]mostbet az casino[/url]
купить диплом техникума недорого [url=educ-ua5.ru]educ-ua5.ru[/url] .
mostbet depozit bonusu [url=https://mostbet4139.ru]https://mostbet4139.ru[/url]
Авто на заказ https://dostavka-avto-russia.ru поиск, диагностика и сопровождение сделки. Машины из Европы, Кореи, Китая и США. Доставка, растаможка и постановка на учёт.
Автомобили на заказ https://dostavka-avto-russia5.ru профессиональный подбор, юридическая проверка, доставка и растаможка. Индивидуальные решения для каждого клиента.
Авто на заказ https://dostavka-avto-russia.ru поиск, диагностика и сопровождение сделки. Машины из Европы, Кореи, Китая и США. Доставка, растаможка и постановка на учёт.
наркологические клиники в москве частные [url=https://narkologicheskaya-klinika-13.ru/]https://narkologicheskaya-klinika-13.ru/[/url] .
Автомобили на заказ https://dostavka-avto-russia5.ru профессиональный подбор, юридическая проверка, доставка и растаможка. Индивидуальные решения для каждого клиента.
Хотите заказать авто https://prignat-avto5.ru Мы подберём оптимальный вариант, проверим машину по базам, организуем доставку и таможенное оформление. Выгодные цены и прозрачные условия.
диплом о среднем образовании купить легально [url=http://www.arus-diplom31.ru]http://www.arus-diplom31.ru[/url] .
mostbet aviator hack [url=http://mostbet4137.ru/]http://mostbet4137.ru/[/url]
построить дом в иркутске [url=stroitelstvo-domov-irkutsk-6.ru]построить дом в иркутске[/url] .
Машины на заказ https://prignat-avto7.ru поиск, диагностика и доставка автомобилей. Индивидуальный подбор, проверенные поставщики и прозрачные условия покупки.
Машины на заказ https://prignat-mashinu5.ru поиск, диагностика и доставка автомобилей. Индивидуальный подбор, проверенные поставщики и прозрачные условия покупки.
Автомобили на заказ https://prignat-mashinu7.ru подбор, проверка, доставка и оформление документов. Машины любых марок и комплектаций с гарантией качества и выгодной ценой.
Машины на заказ https://prignat-avto7.ru поиск, диагностика и доставка автомобилей. Индивидуальный подбор, проверенные поставщики и прозрачные условия покупки.
Машины на заказ https://prignat-mashinu5.ru поиск, диагностика и доставка автомобилей. Индивидуальный подбор, проверенные поставщики и прозрачные условия покупки.
Автомобили на заказ https://prignat-mashinu7.ru подбор, проверка, доставка и оформление документов. Машины любых марок и комплектаций с гарантией качества и выгодной ценой.
мост бет [url=https://mostbet4163.ru]мост бет[/url]
mostbet aviator təlimat [url=http://mostbet4136.ru]http://mostbet4136.ru[/url]
mostbet az etibarlıdırmı [url=http://mostbet4138.ru]http://mostbet4138.ru[/url]
Ремонт квартир https://remontkomand.kz и домов под ключ: дизайн-проект, отделка, инженерные работы. Работаем по договору, фиксированные сроки и цены. Гарантия качества и полный контроль этапов.
mostbet poker otağı [url=www.mostbet4140.ru]mostbet poker otağı[/url]
Ремонт квартир https://remontkomand.kz и домов под ключ: дизайн-проект, отделка, инженерные работы. Работаем по договору, фиксированные сроки и цены. Гарантия качества и полный контроль этапов.
mostbet qeydiyyat [url=https://mostbet4139.ru]https://mostbet4139.ru[/url]
платная наркологическая клиника в москве [url=https://narkologicheskaya-klinika-13.ru/]narkologicheskaya-klinika-13.ru[/url] .
мостбет зеркало скачать [url=http://mostbet4152.ru]http://mostbet4152.ru[/url]
Цены на ремонт https://remontkomand.kz/ru/price квартир и помещений в Алматы под ключ. Узнайте точные расценки на все виды работ — от демонтажа до чистовой отделки. Посчитайте стоимость своего ремонта заранее и убедитесь в нашей прозрачности. Никаких «сюрпризов» в итоговой смете!
купить диплом легальный о высшем образовании [url=www.arus-diplom34.ru]www.arus-diplom34.ru[/url] .
мостбет приложение для android [url=www.mostbet4162.ru]www.mostbet4162.ru[/url]
Купить диплом ВУЗа!
Мы предлагаемвыгодно купить диплом, который выполняется на бланке ГОЗНАКа и заверен мокрыми печатями, водяными знаками, подписями должностных лиц. Данный диплом пройдет лубую проверку, даже при помощи профессиональных приборов. Достигайте свои цели быстро и просто с нашим сервисом- [url=http://techvervellc.com/companies/aurus-diplomany/]techvervellc.com/companies/aurus-diplomany[/url]
купить аттестат за 11 классов госзнак [url=www.arus-diplom25.ru]купить аттестат за 11 классов госзнак[/url] .
mostbet mobil tətbiqi [url=https://mostbet4136.ru]https://mostbet4136.ru[/url]
каталог домов под ключ иркутск [url=http://stroitelstvo-domov-irkutsk-1.ru/]http://stroitelstvo-domov-irkutsk-1.ru/[/url] .
SEO-продвижение сайтов https://raskrutka-sajtov-bystro77.ru в Москве: вывод в ТОП поисковиков, рост трафика и заявок. Полный комплекс — аудит, семантика, оптимизация, ссылки. Эффективное продвижение под ключ.
SEO-продвижение сайтов https://raskrutka-sajtov-bystro77.ru в Москве: вывод в ТОП поисковиков, рост трафика и заявок. Полный комплекс — аудит, семантика, оптимизация, ссылки. Эффективное продвижение под ключ.
mostbet haqqında rəylər [url=https://mostbet4138.ru/]https://mostbet4138.ru/[/url]
Планируете ремонт https://remontkomand.kz в Алматы и боитесь скрытых платежей? Опубликовали полный и честный прайс-лист! Узнайте точные расценки на все виды работ — от демонтажа до чистовой отделки. Посчитайте стоимость своего ремонта заранее и убедитесь в нашей прозрачности. Никаких «сюрпризов» в итоговой смете!
купить диплом о высшем образовании с занесением в реестр цена [url=arus-diplom31.ru]купить диплом о высшем образовании с занесением в реестр цена[/url] .
диплом настоящий купить с занесением в реестр [url=https://www.arus-diplom35.ru]https://www.arus-diplom35.ru[/url] .
диплом купить реестр [url=www.arus-diplom31.ru]диплом купить реестр[/url] .
купить диплом о среднем специальном образовании [url=http://educ-ua2.ru]купить диплом о среднем специальном образовании[/url] .
цветочный горшок высокий напольный купить [url=http://kashpo-napolnoe-moskva.ru/]http://kashpo-napolnoe-moskva.ru/[/url] .
Планируете ремонт https://remontkomand.kz в Алматы и боитесь скрытых платежей? Опубликовали полный и честный прайс-лист! Узнайте точные расценки на все виды работ — от демонтажа до чистовой отделки. Посчитайте стоимость своего ремонта заранее и убедитесь в нашей прозрачности. Никаких «сюрпризов» в итоговой смете!
купить диплом в екатеринбург реестр [url=http://www.arus-diplom33.ru]купить диплом в екатеринбург реестр[/url] .
купить проведенный диплом всеми [url=https://arus-diplom32.ru/]купить проведенный диплом всеми[/url] .
купить аттестат за 11 класс с занесением в реестр в новосибирске [url=http://arus-diplom24.ru]купить аттестат за 11 класс с занесением в реестр в новосибирске[/url] .
Онлайн-курсы Sharewood курсы. Изучайте языки, IT, дизайн, маркетинг и другие направления. Удобный формат, доступ к материалам 24/7
купить диплом сколько [url=educ-ua5.ru]купить диплом сколько[/url] .
купить диплом вуза занесением реестр [url=http://assa0.myqip.ru/?1-4-0-00006201-000-0-0-1752570834]купить диплом вуза занесением реестр[/url] .
купить диплом о высшем образовании украины [url=educ-ua1.ru]купить диплом о высшем образовании украины[/url] .
купить диплом о высшем образовании с занесением в реестр в москве [url=http://www.arus-diplom31.ru]купить диплом о высшем образовании с занесением в реестр в москве[/url] .
Мы готовы предложить документы институтов, которые находятся в любом регионе России. Приобрести диплом о высшем образовании:
[url=http://u-stella.wiki/index.php/Где_Можно_Купить_Аттестат_9_Класс./]купить аттестат 11 класс 2006 год[/url]
купить диплом занесенный реестр [url=https://www.arus-diplom35.ru]купить диплом занесенный реестр[/url] .
аттестат купить 11 кл [url=http://www.arus-diplom23.ru]аттестат купить 11 кл[/url] .
Строительство домов https://stroycata1og.ru и коттеджей под ключ. Готовые проекты, индивидуальные решения, качественные материалы и полный цикл работ — от фундамента до отделки.
Строительство домов https://stroycata1og.ru и коттеджей под ключ. Готовые проекты, индивидуальные решения, качественные материалы и полный цикл работ — от фундамента до отделки.
Журнал о саде https://nasha-gryadka.ru и огороде онлайн — статьи о выращивании овощей, цветов и фруктов. Советы по уходу, борьбе с вредителями, подбору семян и организации участка.
Журнал о саде https://nasha-gryadka.ru и огороде онлайн — статьи о выращивании овощей, цветов и фруктов. Советы по уходу, борьбе с вредителями, подбору семян и организации участка.
онлайн займы быстрый займ
онлайн деньги заем
Нужна качественная регулировка окон пвх? Специалисты настроят створки, фурнитуру и уплотнители. Устранение продувания, перекоса и тяжёлого открывания с гарантией качества.
стп столбовая трансформаторная подстанция [url=http://www.transformatornye-podstancii-kupit2.ru]http://www.transformatornye-podstancii-kupit2.ru[/url] .
прогнозы на спорт бесплатно от профессионалов [url=http://www.prognozy-na-sport-7.ru]http://www.prognozy-na-sport-7.ru[/url] .
наркологические услуги [url=https://narkologicheskaya-klinika-14.ru]https://narkologicheskaya-klinika-14.ru[/url] .
аттестат за 11 классов купить в кемерово [url=www.arus-diplom25.ru/]аттестат за 11 классов купить в кемерово[/url] .
комплектная трансформаторная подстанция купить [url=https://www.transformatornye-podstancii-kupit.ru]https://www.transformatornye-podstancii-kupit.ru[/url] .
прогнозы на хоккей на сегодня [url=https://www.prognozy-na-khokkej.ru]прогнозы на хоккей на сегодня[/url] .
прогнозы на хоккей с подробным анализом [url=https://www.luchshie-prognozy-na-khokkej14.ru]https://www.luchshie-prognozy-na-khokkej14.ru[/url] .
Tree removal and care https://www.highqualitytreeservice.com/ pruning, crown shaping, treatment, removal and felling of hazardous trees. Experienced specialists and modern equipment. Safe, professional and with a guarantee of results.
силовые трансформаторные подстанции [url=www.transformatornye-podstancii-kupit1.ru/]www.transformatornye-podstancii-kupit1.ru/[/url] .
классы аппаратов узи [url=kupit-uzi-apparat25.ru]kupit-uzi-apparat25.ru[/url] .
силовые трансформаторные подстанции [url=http://www.transformatornye-podstancii-kupit2.ru]силовые трансформаторные подстанции[/url] .
можно ли купить в школе аттестат за 11 класс [url=http://arus-diplom21.ru]http://arus-diplom21.ru[/url] .
Мы изготавливаем дипломы любых профессий по выгодным ценам. Заказ диплома, который подтверждает окончание ВУЗа, – это разумное решение. Приобрести диплом любого университета: [url=http://zambianhome.com/author/rochellegaa962/]zambianhome.com/author/rochellegaa962[/url]
диплом купить в реестре [url=https://www.arus-diplom31.ru]диплом купить в реестре[/url] .
Нужен клининг? список клининговых компаний москвы. Лучшие сервисы уборки квартир, домов и офисов. Сравнение услуг, цен и отзывов, чтобы выбрать надежного подрядчика.
Нужен клининг? топ клининговых компаний москвы 2026. Лучшие сервисы уборки квартир, домов и офисов. Сравнение услуг, цен и отзывов, чтобы выбрать надежного подрядчика.
Нужен клининг? лучшие клининговые компании в москве 2026 год. Лучшие сервисы уборки квартир, домов и офисов. Сравнение услуг, цен и отзывов, чтобы выбрать надежного подрядчика.
Стоматологическая клиника https://almazdental35.ru с индивидуальным подходом. Безболезненное лечение, эстетическая стоматология, имплантация и профессиональная гигиена полости рта.
У детей пробелмы с зубами? консультация детского ортодонта — лечение и профилактика зубов у детей. Безопасные методы, комфортная атмосфера и заботливые врачи для маленьких пациентов.
Смотрите сериалы Лучшие сериалы онлайн: https://obzor.city/texty/infotech/onlajn-kinoteatr-lordseries онлайн в хорошем качестве. Новинки, классика и популярные проекты в удобном формате. Бесплатный просмотр без скачивания и доступ 24/7.
Смотрите сериалы Лучшие сериалы онлайн: https://kineshemec.ru/news/obshhestvo-zhizn/serialy-2025-goda-dla-vechera-doma-smotret-onlajn-v-hd-kachestve-51046.html онлайн в хорошем качестве. Новинки, классика и популярные проекты в удобном формате. Бесплатный просмотр без скачивания и доступ 24/7.
прогнозы на спорт хоккей [url=https://luchshie-prognozy-na-khokkej14.ru/]прогнозы на спорт хоккей[/url] .
ставки на хоккей [url=www.prognozy-na-khokkej.ru/]ставки на хоккей[/url] .
купить кашпо для цветов напольное высокое пластиковое [url=http://kashpo-napolnoe-krasnodar.ru/]купить кашпо для цветов напольное высокое пластиковое[/url] .
ставки и прогнозы на спорт [url=https://prognozy-na-sport-8.ru/]https://prognozy-na-sport-8.ru/[/url] .
Нужна контекстная реклама? контекстная реклама для стоматологии под ключ. Настройка в Яндекс.Директ и Google Ads, оптимизация объявлений и контроль заявок.
купить диплом о высшем образовании с занесением в реестр в калуге [url=arus-diplom32.ru]купить диплом о высшем образовании с занесением в реестр в калуге[/url] .
узи прибор [url=www.kupit-uzi-apparat26.ru]узи прибор[/url] .
Нужна контекстная реклама? https://reklama-stomatolog-kontekst.ru под ключ. Настройка в Яндекс.Директ и Google Ads, оптимизация объявлений и контроль заявок.
купить диплом с занесением в реестр самара [url=http://xn--d1abdw2b.net/forum/user/29803/]http://xn--d1abdw2b.net/forum/user/29803/[/url] .
купить аппарат узи цены новый [url=https://kupit-uzi-apparat25.ru/]kupit-uzi-apparat25.ru[/url] .
трансформаторные подстанции столбового типа [url=www.transformatornye-podstancii-kupit1.ru]www.transformatornye-podstancii-kupit1.ru[/url] .
Комплексные IT-решения https://eclat.moscow для бизнеса: разработка, внедрение, сопровождение и поддержка. Надежные технологии для автоматизации и цифровой трансформации.
Комплексные IT-решения https://eclat.moscow для бизнеса: разработка, внедрение, сопровождение и поддержка. Надежные технологии для автоматизации и цифровой трансформации.
букмекерская контора кыргызстан [url=https://mostbet4121.ru]букмекерская контора кыргызстан[/url]
mostbet вход в личный кабинет [url=https://mostbet4120.ru/]mostbet вход в личный кабинет[/url]
мостбет сайт вход [url=https://mostbet4124.ru/]мостбет сайт вход[/url]
Play puzzles online https://plexuspuzzles.com/ free and without restrictions. A huge selection of pictures, simple controls and the ability to develop attention, memory and thinking. A great way to relax and spend time usefully.
mostbet bet [url=http://mostbet4123.ru/]http://mostbet4123.ru/[/url]
мостбет контакты [url=http://mostbet4127.ru]http://mostbet4127.ru[/url]
mostbet бетгеймс [url=https://www.mostbet4122.ru]https://www.mostbet4122.ru[/url]
купить диплом высшее сколько [url=http://www.educ-ua5.ru]купить диплом высшее сколько[/url] .
высшее образование купить диплом с занесением в реестр [url=https://arus-diplom34.ru]высшее образование купить диплом с занесением в реестр[/url] .
купить диплом о высшем образовании в днепропетровске [url=www.educ-ua4.ru/]купить диплом о высшем образовании в днепропетровске[/url] .
теннис букмекерская скачать [url=https://mostbet4125.ru/]https://mostbet4125.ru/[/url]
mostbet official [url=http://mostbet4121.ru/]http://mostbet4121.ru/[/url]
букмекер кыргызстан [url=www.mostbet4120.ru]www.mostbet4120.ru[/url]
купить диплом москва с занесением в реестр [url=http://www.arus-diplom33.ru]купить диплом москва с занесением в реестр[/url] .
мостбет мобильная версия [url=https://mostbet4127.ru/]https://mostbet4127.ru/[/url]
Мы изготавливаем дипломы любой профессии по приятным ценам. Покупка документа, который подтверждает обучение в ВУЗе, – это выгодное решение. Купить диплом любого ВУЗа: [url=http://forum.artinvestment.ru/member.php?u=1807451/]forum.artinvestment.ru/member.php?u=1807451[/url]
купить проведенный диплом в красноярске [url=http://arus-diplom31.ru/]http://arus-diplom31.ru/[/url] .
мостбет официальный сайт [url=https://mostbet4119.ru/]мостбет официальный сайт[/url]
купить аттестаты за 11 класс отзывы москва [url=https://www.arus-diplom25.ru]купить аттестаты за 11 класс отзывы москва[/url] .
купить аттестат за 11 классов с занесением в реестр [url=www.arus-diplom23.ru]купить аттестат за 11 классов с занесением в реестр[/url] .
мостбет регистрация [url=http://mostbet4123.ru]мостбет регистрация[/url]
казино мосбет [url=http://mostbet4124.ru/]http://mostbet4124.ru/[/url]
мостбет официальный сайт вход букмекерская контора [url=http://mostbet4125.ru]http://mostbet4125.ru[/url]
купить проведенный диплом спб [url=http://arus-diplom31.ru]http://arus-diplom31.ru[/url] .
интернет продвижение москва [url=www.internet-agentstvo-prodvizhenie-sajtov-seo.ru]интернет продвижение москва[/url] .
мостбет ком [url=https://mostbet4126.ru]https://mostbet4126.ru[/url]
продвижение сайтов интернет магазины в москве [url=http://poiskovoe-prodvizhenie-sajta-v-internete-moskva.ru/]http://poiskovoe-prodvizhenie-sajta-v-internete-moskva.ru/[/url] .
комплектная трансформаторная подстанция купить [url=dimitrov.forum24.ru/?1-8-0-00000222-000-0-0]комплектная трансформаторная подстанция купить[/url] .
интернет агентство продвижение сайтов сео [url=kompanii-zanimayushchiesya-prodvizheniem-sajtov.ru]kompanii-zanimayushchiesya-prodvizheniem-sajtov.ru[/url] .
ставки мостбет [url=https://www.mostbet4119.ru]https://www.mostbet4119.ru[/url]
кашпо под цветы напольные [url=https://kashpo-napolnoe-krasnodar.ru/]кашпо под цветы напольные[/url] .
компании занимающиеся продвижением сайтов [url=https://poiskovoe-prodvizhenie-moskva-professionalnoe.ru/]компании занимающиеся продвижением сайтов[/url] .
купить аттестат о среднем образовании [url=https://educ-ua2.ru/]купить аттестат о среднем образовании[/url] .
Мы готовы предложить документы учебных заведений, которые расположены в любом регионе России. Купить диплом ВУЗа:
[url=http://alik.forumrpg.ru/viewtopic.php?id=12441#p288129/]купить аттестаты за 11 класс 2021 цена[/url]
раскрутка сайта москва [url=internet-prodvizhenie-moskva.ru]раскрутка сайта москва[/url] .
Приобрести диплом о высшем образовании!
Наша компания предлагаетбыстро и выгодно купить диплом, который выполняется на бланке ГОЗНАКа и заверен мокрыми печатями, штампами, подписями. Наш документ пройдет лубую проверку, даже при использовании специально предназначенного оборудования. Решите свои задачи быстро с нашей компанией- [url=http://sz.80lvl.ru/viewtopic.php?f=9&t=11047/]sz.80lvl.ru/viewtopic.php?f=9&t=11047[/url]
сайт мостбет [url=www.mostbet4130.ru]www.mostbet4130.ru[/url]
swot анализ swot анализ выявляет
mostbet website [url=http://mostbet4129.ru]http://mostbet4129.ru[/url]
Мы изготавливаем дипломы любых профессий по приятным тарифам. Купить диплом техникума — [url=http://kyc-diplom.com/diplom-tekhnikuma.html/]kyc-diplom.com/diplom-tekhnikuma.html[/url]
seo продвижение и раскрутка сайта [url=http://internet-agentstvo-prodvizhenie-sajtov-seo.ru/]seo продвижение и раскрутка сайта[/url] .
купить диплом занесением реестр украины [url=http://uralmotoclub.ru/profile/vadyymemelnvv]купить диплом занесением реестр украины[/url] .
мостбет промокод на бонус [url=http://mostbet4169.ru/]http://mostbet4169.ru/[/url]
купить диплом о высшем образовании бакалавр [url=educ-ua18.ru]купить диплом о высшем образовании бакалавр[/url] .
фабрика по производству одежды [url=http://www.nitkapro.ru]http://www.nitkapro.ru[/url] .
mostbet mobile [url=mostbet4165.ru]mostbet mobile[/url]
mostbet uz futbol tikish [url=mostbet4167.ru]mostbet4167.ru[/url]
интернет продвижение москва [url=http://internet-prodvizhenie-moskva.ru]интернет продвижение москва[/url] .
Мы готовы предложить документы университетов, расположенных в любом регионе Российской Федерации. Заказать диплом о высшем образовании:
[url=http://mbableu.com/employer/ukrdiplom/]купить аттестат в челябинске за 11 класс[/url]
комплектная трансформаторная подстанция купить [url=https://turforum.borda.ru/?1-8-0-00003432-000-0-0-1756370353]комплектная трансформаторная подстанция купить[/url] .
мостбет официальный сайт регистрация [url=https://mostbet4129.ru]https://mostbet4129.ru[/url]
мостбет уз скачать [url=http://mostbet4130.ru]http://mostbet4130.ru[/url]
узи аппарат цена новый [url=https://kupit-uzi-apparat27.ru]узи аппарат цена новый[/url] .
Приобрести диплом на заказ в Москве можно используя официальный сайт компании. [url=http://aytokariyer.com.tr/employer/diploms-ukraine/]aytokariyer.com.tr/employer/diploms-ukraine[/url]
ставки мостбет [url=http://mostbet4128.ru/]http://mostbet4128.ru/[/url]
поисковое продвижение сайта в интернете москва [url=http://internet-agentstvo-prodvizhenie-sajtov-seo.ru/]поисковое продвижение сайта в интернете москва[/url] .
mostbet for iphone [url=http://mostbet4166.ru/]http://mostbet4166.ru/[/url]
частный seo оптимизатор [url=https://poiskovoe-prodvizhenie-sajta-v-internete-moskva.ru/]https://poiskovoe-prodvizhenie-sajta-v-internete-moskva.ru/[/url] .
mostbet official [url=www.mostbet4128.ru]mostbet official[/url]
купить диплом с занесением в реестр в иркутске [url=https://arus-diplom31.ru/]купить диплом с занесением в реестр в иркутске[/url] .
ЭВЛО https://evlo-phlebology.ru эндовазальная лазерная коагуляция вен, наряду со склеротерапией является эффективным методом лечения варикозного расширения вен на ногах.
Услуги госпитализации https://hospitall.ru экстренная помощь при угрожающих состояниях и плановое лечение с заранее согласованной программой. Подбор клиники, транспортировка и поддержка пациента на всех этапах.
Looking for second-hand? thrifting near me We have collected the best stores with clothes, shoes and accessories. Large selection, unique finds, brands at low prices. Convenient catalog and up-to-date contacts.
продвижение сайта [url=https://internet-agentstvo-prodvizhenie-sajtov-seo.ru/]продвижение сайта[/url] .
купить диплом занесением реестр отзывы [url=https://arus-diplom33.ru]купить диплом занесением реестр отзывы[/url] .
цифровой маркетинг статьи [url=http://statyi-o-marketinge.ru]http://statyi-o-marketinge.ru[/url] .
мостбет скачать андроид [url=http://mostbet4155.ru/]мостбет скачать андроид[/url]
mostbet for pc [url=http://mostbet4154.ru]mostbet for pc[/url]
купить свидетельство о рождении ребенка [url=www.educ-ua5.ru]www.educ-ua5.ru[/url] .
купить диплом занесением в реестр [url=http://educ-ua12.ru]купить диплом занесением в реестр[/url] .
мостбет мобильная версия скачать [url=https://www.mostbet4157.ru]https://www.mostbet4157.ru[/url]
быстрая регистрация на мостбет [url=http://mostbet4158.ru]http://mostbet4158.ru[/url]
доставка из китая в москву дешевая доставка из китая в россию
фермерская продукция интернет магазин фермерских продуктов с доставкой
скачать мостбет казино на андроид [url=https://mostbet4160.ru/]https://mostbet4160.ru/[/url]
мостбет лицензия [url=mostbet4156.ru]mostbet4156.ru[/url]
наркология клиника [url=www.narkologicheskaya-klinika-11.ru]www.narkologicheskaya-klinika-11.ru[/url] .
мостбет казино войти [url=http://mostbet4155.ru]http://mostbet4155.ru[/url]
ljv gjl rk.x [url=www.stroitelstvo-domov-irkutsk-2.ru/]www.stroitelstvo-domov-irkutsk-2.ru/[/url] .
наркологическая клиника в москве [url=https://www.narkologicheskaya-klinika-12.ru]https://www.narkologicheskaya-klinika-12.ru[/url] .
мостбет ставки на исход [url=www.mostbet4154.ru]мостбет ставки на исход[/url]
monsbet [url=www.mostbet4159.ru]www.mostbet4159.ru[/url]
Надежная доставка из китая в Россию: от документов до контейнеров. Выбираем оптимальный маршрут, оформляем таможню, страхуем грузы. Контроль сроков и сохранность на каждом этапе.
руководства по seo [url=https://statyi-o-marketinge2.ru/]https://statyi-o-marketinge2.ru/[/url] .
мосвет казино [url=https://mostbet4153.ru/]https://mostbet4153.ru/[/url]
mostbet mobile [url=www.mostbet4157.ru]mostbet mobile[/url]
заказать сайт на тильде https://www.art-made.ru
Надежная доставка грузов из китая: от небольших партий до контейнеров. Авиа, морем, авто и железной дорогой. Оформление, страхование и логистика в кратчайшие сроки.
Нужен автобусный билет? заказ билетов на автобус онлайн просто и удобно. Поиск рейсов, сравнение цен, выбор мест и моментальная оплата. Актуальное расписание, надежные перевозчики и выгодные тарифы каждый день.
мост бет букмекерская контора [url=www.mostbet4159.ru]www.mostbet4159.ru[/url]
материалы по маркетингу [url=http://statyi-o-marketinge.ru]http://statyi-o-marketinge.ru[/url] .
Качественный ремонт квартир https://expertremonta.kz от Компании «Эксперт ремонта» это качественный ремонт квартир под ключ в Алматы. Выбирайте Эксперт Ремонта — тут бесплатный выезд замерщика, официальные документы, гарантия документально, ремонт квартир без предоплаты.
доставка топлива доставка дизельного топлива по московской области
купить грунт оптом чернозем купить с доставкой
mostbet официальный сайт вход [url=http://mostbet4158.ru/]http://mostbet4158.ru/[/url]
Мобильный выездной шиномонтаж https://master-shin.by круглосуточная помощь в дороге. Экстренная помощь в дороге может понадобиться каждому автолюбителю, и наша компания оказывает ее на высочайшем профессиональном уровне, на самых выгодных в Минске условиях. Оперативный выезд по городу и области, доступные и полностью адекватные цены, квалифицированная сервисная и консультационная поддержка, круглосуточное реагирование, вне зависимости от погодных условий.
Ремонт ноутбуков https://01km.ru телефонов, телевизоров, принтеров и компьютеров в Одинцово и Москве.
go to the website online: https://saffronholidays.in
mostbe [url=http://mostbet4153.ru]http://mostbet4153.ru[/url]
visit our website: https://www.acuam.com
the best site for you: https://telrad.com
our site is waiting for you: https://hyundaimobil.co.id
купить диплом о среднем техническом образовании [url=www.educ-ua2.ru/]купить диплом о среднем техническом образовании[/url] .
купить диплом о высшем образовании в николаеве [url=http://educ-ua5.ru]купить диплом о высшем образовании в николаеве[/url] .
купить легально диплом [url=www.educ-ua14.ru/]купить легально диплом[/url] .
our new official website: https://girls-media.com
I found a cool site: https://underatexassky.com
Mochten Sie ein hauser in Montenegro kaufen kaufen? Tolle Angebote am Meer und in den Bergen. Gro?e Auswahl an Immobilien, Unterstutzung bei der Immobilienauswahl, Transaktionsunterstutzung und Registrierung. Leben Sie in einem Land mit mildem Klima und wunderschoner Natur.
сколько стоит купить аттестат 11 класса [url=www.educ-ua18.ru/]сколько стоит купить аттестат 11 класса[/url] .
русское порно молодых русское порно мжм
Want to have fun? hack apk Watch porn, buy heroin or ecstasy. Pick up whores or buy marijuana. Come in, we’re waiting
Новые актуальные промокоды iherb 2025 для выгодных покупок! Скидки на витамины, БАДы, косметику и товары для здоровья. Экономьте до 30% на заказах, используйте проверенные купоны и наслаждайтесь выгодным шопингом.
Мы предлагаем документы институтов, расположенных в любом регионе Российской Федерации. Приобрести диплом о высшем образовании:
[url=http://jobbid.org/employer/all-diplomy/]купить аттестат за 11 класс в ростове на дону[/url]
наркологическая частная клиника [url=https://narkologicheskaya-klinika-13.ru/]https://narkologicheskaya-klinika-13.ru/[/url] .
где можно купить диплом о высшем образовании [url=http://educ-ua3.ru]где можно купить диплом о высшем образовании[/url] .
платный наркологический диспансер москва [url=www.narkologicheskaya-klinika-14.ru/]www.narkologicheskaya-klinika-14.ru/[/url] .
сколько стоит купить диплом специалиста [url=http://educ-ua17.ru/]сколько стоит купить диплом специалиста[/url] .
mostbet azerbaycan [url=https://mostbet4142.ru/]https://mostbet4142.ru/[/url]
play puzzles online: https://www.reddit.com/user/ornery-conference515/
mostbet mobil giriş [url=mostbet4141.ru]mostbet4141.ru[/url]
Самое лучшее в сети: https://poloniya.ru
The most useful information: https://satapornbooks.com
mostbet mobil giriş [url=www.mostbet4144.ru]www.mostbet4144.ru[/url]
доставка из китая карго доставка из китая в россию цена
шпонирование фанеры производство шпона
геодезист москва геодезические изыскания москва цена
геотекстиль 600 купить геотекстиль для пруда
блог интернет-маркетинга [url=www.blog-o-marketinge1.ru/]блог интернет-маркетинга[/url] .
Включение в реестр Минпромторга https://minprom-info.ru официальный путь для подтверждения отечественного производства. Подготовка и подача документов, юридическое сопровождение и консультации для производителей.
Занятия по самообороне https://safety-skills.ru практические навыки защиты в реальных ситуациях, развитие силы и выносливости. Профессиональные тренеры помогут освоить приемы борьбы, удары и тактику безопасности.
Платформа онлайн-обучения https://craftsmm.ru курсы по маркетингу, продажам и рекламе для новичков и профессионалов. Освойте современные инструменты продвижения, увеличьте продажи и развивайте карьеру в удобном формате.
Написание дипломов на заказ https://vasdiplom.ru помощь студентам в подготовке итоговых работ. Авторские тексты, проверка на уникальность и полное соответствие стандартам учебных заведений.
mostbet qeydiyyat zamanı bonus [url=http://mostbet4141.ru/]http://mostbet4141.ru/[/url]
visit our best site online: https://iclei.org
The best we have here: https://cour-interieure.fr
mostbet az slotlar [url=https://mostbet4142.ru]https://mostbet4142.ru[/url]
Выгодно купить диплом любого института!
Мы готовы предложить дипломы психологов, юристов, экономистов и других профессий по доступным тарифам— [url=http://humanitariancollege.ru/]humanitariancollege.ru[/url]
mostbet parolni unutdingizmi [url=http://mostbet4171.ru/]mostbet parolni unutdingizmi[/url]
купить диплом недорого [url=http://educ-ua19.ru]купить диплом недорого[/url] .
купить диплом специалиста дешево [url=https://educ-ua18.ru/]купить диплом специалиста дешево[/url] .
The latest information is here: https://unilago.com
We have the latest information: https://fish-pet.com
visit our website: https://cere-india.org
We are waiting for you on the site: https://travel2mv.com
mostbet az giriş bloku [url=https://mostbet4140.ru]https://mostbet4140.ru[/url]
обучение seo [url=www.kursy-seo-2.ru]обучение seo[/url] .
обучение seo [url=http://kursy-seo-1.ru/]http://kursy-seo-1.ru/[/url] .
seo с нуля [url=kursy-seo-1.ru]kursy-seo-1.ru[/url] .
seo интенсив [url=https://kursy-seo-4.ru/]kursy-seo-4.ru[/url] .
блог seo агентства [url=https://statyi-o-marketinge2.ru]https://statyi-o-marketinge2.ru[/url] .
seo онлайн [url=http://kursy-seo-3.ru]http://kursy-seo-3.ru[/url] .
mostbet qanunidirmi [url=https://mostbet4144.ru]https://mostbet4144.ru[/url]
mostbetin [url=http://mostbet4171.ru/]http://mostbet4171.ru/[/url]
New and relevant information: https://amt-games.com
The best of our site: https://www.feldbahn-ffm.de
Want to have fun? melbet drugs Whores, drugs, casino. We have it all, any drugs are on sale.
порно старых шлюхи ххх
Обучение и семинары https://uofs-beslan.ru для профессионалов: современные программы, практические кейсы и опыт экспертов. Развивайте навыки, повышайте квалификацию и получайте новые возможности для карьерного роста.
Академия парикмахерского искусства https://charm-academy.ru обучение от ведущих мастеров. Современные техники стрижек, окрашивания и укладок. Курсы для начинающих и профессионалов с практикой и дипломом по окончании.
Лицей взаимного обучения https://talgenisty.ru уникальная среда для детей и взрослых. Совместные уроки, обмен опытом, мастер-классы и творческие проекты. Образование, основанное на поддержке и сотрудничестве.
Школа видеорекламы https://tatyanamostseeva.ru обучение созданию креативных роликов для бизнеса и брендов. Практические занятия, работа с современными инструментами и поддержка экспертов. Освойте профессию в сфере digital.
The best site for you: https://www.acuam.com
Great site for everyone: https://www.europneus.es
Приём макулатуры https://chsreda.ru в Казани работает как для частных лиц, так и для организаций. Сдают газеты, журналы, картонные коробки, офисную бумагу. Это реально удобно, потому что приезжают, забирают прямо с территории, а потом всё идёт на переработку.
Кухонные принадлежности https://www.kitchen-store.ru в магазине для дома: современная посуда, полезные гаджеты, текстиль и аксессуары. Стильные решения для кухни, выгодные цены и большой ассортимент.
Нужен автобусный билет? купить билет на автобус удобный сервис поиска и бронирования. Широкий выбор направлений, надежные перевозчики, доступные цены и моментальная отправка электронных билетов на почту.
Автомобильный портал https://auto-club.pl.ua онлайн-площадка для автолюбителей. Подробные обзоры машин, тест-драйвы, свежие новости, советы по ремонту и обслуживанию. Удобный поиск и актуальные материалы.
Авто портал https://diesel.kyiv.ua все о мире автомобилей: новости, обзоры моделей, тест-драйвы, советы по выбору и уходу за авто. Каталог машин, актуальные цены, автоуслуги и полезная информация для автовладельцев.
Все для автомобилистов https://k-moto.com.ua на авто портале: новости, обзоры, статьи, каталоги и цены на автомобили. Экспертные мнения, тест-драйвы и практические советы по эксплуатации авто.
игра авиатор ставки [url=aviator-igra-3.ru]игра авиатор ставки[/url] .
Нужна виза? оформление венгерской визы Консультации, подготовка документов, сопровождение на всех этапах. Визы в Европу, США, Азию и другие страны. Доступные цены и надежная поддержка.
Онлайн женский портал https://elegance.kyiv.ua актуальные советы по красоте, стилю, кулинарии и семейной жизни. Разделы о здоровье, карьере и саморазвитии. Интересные статьи и общение с единомышленницами.
Портал для женщин https://fashionadvice.kyiv.ua сайт для девушек и женщин, которые ценят красоту, уют и гармонию. Советы по стилю, отношениям, материнству и здоровью. Читайте статьи, делитесь опытом и вдохновляйтесь новыми идеями.
Женский портал https://beautyadvice.kyiv.ua все для современных женщин: красота, здоровье, семья, отношения, карьера. Полезные статьи, советы экспертов, лайфхаки и вдохновение каждый день. Онлайн-сообщество для общения и развития.
диплом об окончании техникума купить [url=https://www.educ-ua9.ru]диплом об окончании техникума купить[/url] .
Купить диплом техникума в Чернигов [url=https://educ-ua8.ru]Купить диплом техникума в Чернигов[/url] .
купить диплом в москве с занесением в реестр [url=www.arus-diplom31.ru/]купить диплом в москве с занесением в реестр[/url] .
Авто портал https://avtoshans.in.ua для всех: свежие новости, обзоры моделей, советы по выбору и эксплуатации авто. Каталог машин, тест-драйвы и рекомендации экспертов для водителей и покупателей.
Автомобильные новости https://reuth911.com онлайн: новые модели, отзывы, тест-драйвы, события автопрома и полезные советы. Узнайте первыми о главных новинках и трендах автомобильного мира.
Портал про автомобили https://myauto.kyiv.ua онлайн-ресурс для автолюбителей. Обзоры, статьи, тест-драйвы, цены и полезные советы по ремонту и уходу за машиной. Всё о мире авто в одном месте.
Свежие новости авто https://orion-auto.com.ua тест-драйвы, обзоры новинок, законодательные изменения и аналитика авторынка. Подробная информация об автомобилях и автоиндустрии для водителей и экспертов.
Мы изготавливаем дипломы любой профессии по доступным тарифам. Купить диплом в Новомосковске — [url=http://kyc-diplom.com/geography/novomoskovsk.html/]kyc-diplom.com/geography/novomoskovsk.html[/url]
сделать проект квартиры для перепланировки [url=proekt-pereplanirovki-kvartiry8.ru]proekt-pereplanirovki-kvartiry8.ru[/url] .
Автомобильный сайтhttps://setbook.com.ua свежие новости, обзоры моделей, тест-драйвы и советы экспертов. Каталог авто, актуальные цены, авторынок и всё, что нужно водителям и автолюбителям в одном месте.
Онлайн-журнал для женщин https://fines.com.ua стиль, уход за собой, психология, рецепты, материнство и карьера. Актуальные материалы, тренды и экспертные рекомендации каждый день.
Онлайн-сайт для женщин https://musicbit.com.ua стиль, уход за собой, психология, семья, карьера и хобби. Интересные статьи, тесты и форум для общения. Пространство для вдохновения и развития.
Женский сайт о жизни https://prettywoman.kyiv.ua секреты красоты, мода, здоровье, рецепты и отношения. Интересные статьи, советы и лайфхаки. Всё, что нужно, чтобы чувствовать себя уверенно и счастливо.
1win официальный [url=http://1win12002.ru/]http://1win12002.ru/[/url]
Онлайн-сайт про автомобили https://tvregion.com.ua свежие новости, аналитика рынка, обзоры и сравнения машин. Советы по обслуживанию и выбору авто. Всё для водителей и автолюбителей в одном месте.
Женский онлайн-журнал https://feminine.kyiv.ua мода, красота, здоровье, отношения и семья. Полезные советы, вдохновляющие статьи, лайфхаки для дома и карьеры. Всё самое интересное для современных женщин.
Автомобильный портал https://troeshka.com.ua онлайн-ресурс для автовладельцев. Каталог машин, тест-драйвы, аналитика авторынка и советы специалистов. Будьте в курсе новинок и технологий автоиндустрии.
Сайт для женщин https://lolitaquieretemucho.com мода, красота, здоровье, отношения, семья и карьера. Полезные советы, статьи, рецепты и лайфхаки. Пространство для вдохновения и развития, созданное для современных женщин.
1 x win [url=http://1win12001.ru]1 x win[/url]
Сайт для женщин https://femaleguide.kyiv.ua гармония стиля и жизни. Уход за собой, рецепты, дом, отношения, карьера и путешествия. Читайте статьи, делитесь опытом и вдохновляйтесь новыми идеями.
Сайт про машины https://tvk-avto.com.ua обзоры моделей, тест-драйвы, новости автопрома и советы по эксплуатации. Полезные статьи о выборе авто, уходе, ремонте и актуальные материалы для автовладельцев.
Автомобильный новостной портал https://tuning-kh.com.ua всё об авто в одном месте: новости, цены, обзоры, тест-драйвы, авторынок. Советы экспертов и полезные материалы для водителей и тех, кто планирует купить машину.
Женский онлайн портал https://femalesecret.kyiv.ua онлайн-ресурс для девушек и женщин. Мода, красота, здоровье, семья и материнство. Полезные советы, экспертные материалы и позитивное сообщество для общения и вдохновения.
mostbet регистрация [url=mostbet12001.ru]mostbet регистрация[/url]
mostbet игры [url=https://mostbet12004.ru/]https://mostbet12004.ru/[/url]
Онлайн-сайт для женщин https://mirlady.kyiv.ua красота, стиль, здоровье, дом и семья. Практичные рекомендации, модные идеи, вдохновение и поддержка. Лучший контент для девушек и женщин любого возраста.
Женский сайт https://lubimoy.com.ua стиль, уход за собой, психология, материнство, работа и хобби. Актуальные статьи, тренды и экспертные советы. Всё самое важное для гармоничной жизни и успеха.
Сайт для женщин https://amideya.com.ua портал о красоте, стиле, здоровье, семье и саморазвитии. Ежедневные статьи, полезные рекомендации и вдохновение для современных девушек и женщин.
Женский онлайн-журнал https://gracefullady.kyiv.ua свежие статьи о моде, красоте, здоровье и саморазвитии. Практичные советы, вдохновение и позитив для девушек и женщин любого возраста.
1win bet [url=https://1win12003.ru/]https://1win12003.ru/[/url]
1хставка лайв [url=http://1win12001.ru/]http://1win12001.ru/[/url]
1win ставки на спорт скачать [url=https://1win12002.ru]https://1win12002.ru[/url]
мостбет. вход. [url=http://mostbet12002.ru]мостбет. вход.[/url]
latest information here: https://astra-hotel.ch
Here is the best on the net: https://www.manaolahawaii.com
visit our website: https://lmc896.org
Latest information from us: https://www.europneus.es
mostbet личный кабинет [url=https://mostbet12004.ru/]mostbet личный кабинет[/url]